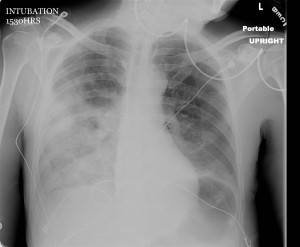
[tab_nav type=”two-up”][tab_nav_item title=”Clinical Case” active=”true”][tab_nav_item title=”Answer” active=””][/tab_nav][tabs][tab active=”true”]A 68 year-old male is brought to the ED from a nursing home with a fever & cough. He has a history of HTN, parkinson’s dementia, DM, and a previous CVA. He is altered and unable to give much of a history, but by report he has had a decreased appetite, coughing up a large amount of dark, bloody sputum, and is now obtunded. His vital signs are as follows: 39.0 142 [84-96] / [45-60] 32 88% on NRB. The patient was intubated for hypoxic respiratory failure. His chest x-ray is below:
What is your diagnosis and what antibiotics should you give?
[/tab][tab]
Diagnosis: Necrotizing pneumonia with lung abscesses
Necrotizing pneumonia is a rare, but potentially deadly complication of bacterial pneumonia.
It is characterized by the finding of pneumonic consolidation with multiple areas of necrosis within the lung parenchyma. Necrotic foci may coalesce, resulting in a localized lung abscess, or pulmonary gangrene if involving an entire lobe.
Most common pathogens: S. aureus, S. pneumoniae, and Klebsiella pneumonia.
- Others include S. epidermidis, E. coli, Acinetobacter baumannii, H. influenzae and Pseudomonas.
- Rarely, anaerobes such as Clostridia species & Bacteroides species are reported.
- S. aureus strains, often methicillin-resistant, that produce cytotoxin Panton–Valentine leukocidin (PVL) are associated with causing progressive & hemorrhagic necrotizing pneumonia – especially in young immunocompetent patients.
- Other studies also suggested that a-hemolysin and possibly other cytotoxins are responsible for the pathogenesis.
- Sputum culture/gram stain, blood cultures, BAL, & plural fluid studies may be helpful, however the overall positive percentage variably ranges between 40 and 100%.
Contrast-enhanced chest CT is the diagnostic test of choice and is also helpful in evaluating for parenchymal complications.
Empiric antibiotic therapy should include:
- Broad spectrum coverage for commonly implicated pathogens (ex: vancomycin, pseudomonal-dose piperacillin/tazobactam).
- ADD clindamycin or metronidazole if chosen primary antimicrobials do not provide anaerobic coverage.
Consider an early surgical evaluation for the patient with necrotizing pneumonia complicated by septic shock, empyema, bronchopleural fistula, or hemoptysis.
Reference
- Tsai YF, Ku YH. Necrotizing pneumonia: a rare complication of pneumonia requiring special consideration. Curr Opin Pulm Med. 2012 May; 18(3):246-52.
[/tab][/tabs]
[author title=”About the Author”]