[tab_nav type=”two-up”][tab_nav_item title=”Clinical Case” active=”true”][tab_nav_item title=”Answer” active=””][/tab_nav][tabs][tab active=”true”]
You are awoken at 0300 by the ICU intern stating that the new admission is in room 11.
En route she tells you all that she knows so far:
“The patient is a 52 yo F brought in to the emergency department by EMS after she was found in extremis by her boyfriend. He states that for the past 3 days she was too short of breath to do anything so he would just bring her food and try to let her rest. Today he arrived to her home and found her pale, confused and diaphoretic. He immediately called 911 who found her to be 60/palp with a HR of 167. They had a hard time getting stable access in the ED so right after the junior resident was finished intubating, the ED senior placed a L IJ TLC. She was taken to the MICU before a CXR could be completed, but the ED team was so confident of the line placement that she was started on pressors, IVF, and broad spectrum antibiotics”
“I questioned the boyfriend when he arrived to the ICU with her and all he knew about her prior health is that she had a lot of surgeries as a baby, but has otherwise been very healthy. I didn’t get a chance to see her yet as the nurses were getting her settled, but her vital signs looked pretty good.”
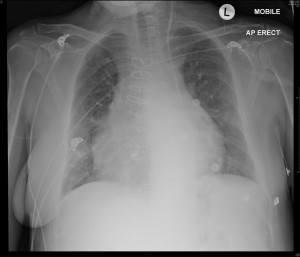
After you wipe the crust from over your eyes you send the intern out to start her initial assessment and you follow at a groggy pace. As you approach the room you see the radiology tech leaving the room and he shows you the CXR he just took:
You panic and run into the room to find a comfortable woman laying there. The intern is an avid Surviving Sepsis fan and hooks up the TLC for a CVP: 13……
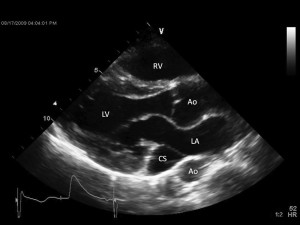
You use an US probe and see the following images:
Courtesy of Wei Xiong link
The question is: What is the explanation for this situation? What do you NEED to do next?
[/tab][tab]
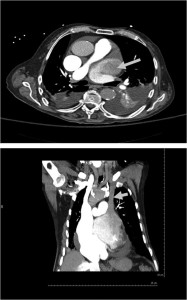
◊ There is a limited differential for left paramediastinal catheters:
- Venous:
- left sided superior vena cava
- left internal mammary vein
- left superior intercostal vein
- left pericardiophrenic vein
- Arterial
- left subclavian artery to descending thoracic aorta
- extravascular position
- it is possible to inadvertently place a line directly into the mediastinum or pleural space
Based on a combination of CXR, echo findings of a dilated coronary sinus (CS), a hemodynamically stable pt with a presumed history of congenital heart disease, and the measurement of low pressures on CVP monitoring, the most likely diagnosis is:
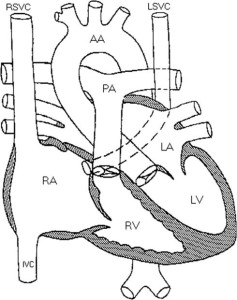
◊ A Persistant Left Superior Vena Cava (PLSVC), the most common congenital venous anomaly in the chest
- 0.3% of general population;
- 4.3-11% of patients with Congenital Heart Disease (CHD)
Chest. 2009;136(2):617-620
◊ There are two types:
- 90% have a left SVC that connects to the right atrium via a dilated coronary sinus, like our patient
- 10% have a connection to the left atrium, usually associated with a small ASD and a minor right-to-left shunt
◊ Most cases (82 – 90%) are associated with a small right sided SVC; additionally, a persistent bridging vein (left brachiocephalic vein) is seen in 25 – 35%
◊ Clinical Presentation is usually asymptomatic, with most cases found incidentally on CT scan or echo. Even with drainage to the left atrium, the return is not usually enough to cause stenosis.
◊ Treatment is usually reserved for treatment of large right-to-left shunts (rare). The true importance comes when working with venous procedures, such as line placement or pacemaker implantation, as failure to recognize this abnormal anatomy can lead to improper placement.
Case Conclusion: The patient did have a Tetralogy of Fallot repair when she was younger (the most common CHD linked to PLSVC). She had a simple septic evaluation showing an advanced pneumonia. Antibiotic treatment was completed and a thorough cardiology evaluation found no signs of shunt via a TEE with bubble. Pt was extubated shortly after admission and discharged home without event.
Suggested Reading
- Thaiyananthan NN, Jacono FJ III, Patel SR, Kern JA, Stoller JK (2009) Right-to-left anatomic shunt associated with a persistent left superior vena cava: the importance of injection site in demonstrating the shunt. Chest 136:617–620.
- Xiong W, Shi C. Concomitant Persistent Left Superior Vena Cava and Agenesis of Right Superior Vena Cava. A Rare Congenital Anomaly. Circulation 2010;121:2329-30.
[/tab][/tabs]