[tab_nav type=”two-up”][tab_nav_item title=”Clinical Case” active=”true”][tab_nav_item title=”Answer” active=””][/tab_nav][tabs][tab active=”true”] A 24 y/o male with a history of bipolar disorder and depression is admitted to your ICU from the Emergency Department after taking approximately 60 – 450mg ER lithium pills an hour prior to presentation in suicide attempt. He is currently vomiting with VS as follows: 37.5 C HR 115 BP: 120’s/70’s RR: 22 SpO2: 99% on RA. His exam is unremarkable and his EKG shows only sinus tachycardia. His initial lithium level in the ED is 3.0 mmol/L.
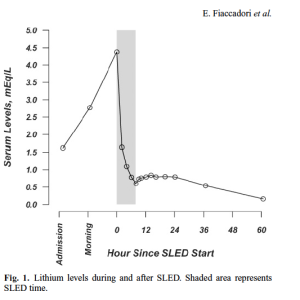
You quickly place an NG tube, start whole bowel irrigation, and put in an right IJ dialysis catheter to prepare the patient for emergent HD. His 2 hour repeat lithium level is 6.6 mmol/L so you decide to start HD. The patient’s 2 & 4 hour levels are down to <1 mmol/L, but the next morning you find his level just jumped back up to 4.0 mmol/L after his HD stopped.
Your friendly nephrologist comes to see the patient and recommends another course of standard hemodialysis followed by 18 hours of CVVHD. What’s the deal?
[/tab][tab]
Lithium Toxicity
- Small molecule (7 Da), low protein binding, water soluble drugs
- One of the dialyzable drugs (“I STUMBLE”)
- Isopropyl Alcohol
- Salycylates
- Theophylline
- Uremia
- Methanol
- Barbiturates, beta-blockers (water soluble, such as atenolol)
- Lithium
- Ethylene glycol
- Lithium pharmacokinetics follow a two compartment model [active drug found in both intra- & extracellular compartment]
- Central compartment: Highly perfused tissues (e.g. blood, extracellular fluid, liver, kidneys, etc.)
- Peripheral compartment: Poorly perfused tissues (e.g. muscle, fat, etc.)
- Causes a reduced GFR and urinary concentrating ability by 15% of normal maximum (Nephrogenic DI)
- Many preparations of lithium are sustained release forms (longer absorption times)
Treatment of Acute Toxicity
- Goal: Prevent and lower intracellular lithium levels
- Consider whole bowel irrigation if the patient who ingested extended release lithium tabs
- Forget activated charcoal – lithium is not absorbed by AC
- Hydrate the patient aggressively to improve renal clearance of lithium (it doesn’t get metabolized)
- Extracorporeal elimination
- Indications
- Renal failure
- Severe neurologic dysfunction
- Inability to tolerate fluid replacement
- Lithium concentration > 4 mmol/L (acute ingestion), >=2.5 mmol/L (chronic ingestion)
- Improvement of clinical symptoms will occur after hemodialysis, however
- After HD, a rebound in serum lithium levels may occur because of the slow diffusion of lithium from the peripheral compartment.
- Indications
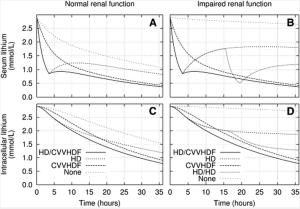
- Hemodialysis: The most effective method for clearing lithium in the extracellular compartment.
- Mode of choice if hemodynamically stable
- Can clear 70-160 mL/min (Normal renal clearance 15-30 mL/min)
- As extracellular clearance occurs, intracellular lithium diffuses along gradient back into extracellular compartment for HD to clear.
- After IHD stops, diffusion of lithium from the gut and from the peripheral compartment will commonly cause a rebound lithium levels 6-10 hours after cessation of IHD – just enough time to think you are in the clear.
- Sustained low-efficiency dialysis (SLED): A longer, slower session of dialysis (6-8 hrs) shown to provide adequate clearance of lithium level – disadvantage is it is still intermittent.
- Continuous veno-venous hemodialysis (CVVHD/CVVHDF): Continuous solute clearance that may be better tolerated by those with hemodynamic collapse (lower Qb’s)
- If CRRT unavailable, strongly consider arranging for a repeat IHD session as you trend serial (q2h) lithium levels should rebound toxicity occur.
References & Resources
- Meertens JH, Jagernath DR, Eleveld DJ, Zijlstra JG, Franssen CF. Haemodialysis followed by continuous veno-venous haemodiafiltration in lithium intoxication; a model and a case. Eur J Intern Med. 2009;20(3):e70-3.
- Fiaccadori E, Maggiore U, Parenti E, et al. Sustained low-efficiency dialysis (SLED) for acute lithium intoxication. NDT Plus 2008 1: 329-332.
- Waring WS. Management of lithium toxicity. Toxicol Rev. 2006;25(4):221-30.
- Life In The Fastlane – Toxicology Conundrums Series
[/tab][/tabs]
[author title=”About the Author”]