[tab_nav type=”two-up”][tab_nav_item title=”Clinical Case” active=”true”][tab_nav_item title=”Answer” active=””][/tab_nav][tabs][tab active=”true”]A 32 y/o male with a history of NICM (LVEF ~ 5%) s/p LVAD placement gets admitted to your ICU with a reported episode of a wide-complex tachycardia. The patient denies chest pain, shortness or breath, nausea or recent vomiting. He initially came to the emergency department because his LVAD control box was alarming – specifically is low flow alarm, but that has since stopped. While you are standing at the bedside, the patient’s rhythm changes to the following:
Question: What is the patient’s diagnosis, and how would you manage this patient?
[/tab][tab]
Managing the Ventricular Arrhythmias in the LVAD patient
Ventricular arrhythmias affect at least 1/3 of all patients with long-term VAD support for advanced heart failure, and most commonly occur within the 1st month after implantation. Ventricular tachydysrhythmias are usually well tolerated, but can cause significant problems if they reduce LV filling – remember, the right ventricle is not being supported by the LVAD! A number of studies have found an increased mortality in patients with VT with a VAD, so it shouldn’t be taken likely.
Proposed etiologies
- Electrical remodeling of cardiac tissue after implantation. QT interval is often prolonged in patients with chronic heart failure, and VADs may worsen QT prolongation by cardiac decompression (contraction-excitation feedback mechanism)
- Myocardial fibrosis after VAD implantation – caused by increased collagen production, fibrotic scar around cannula resulting in re-entry circuits, & cellular hypertrophy.
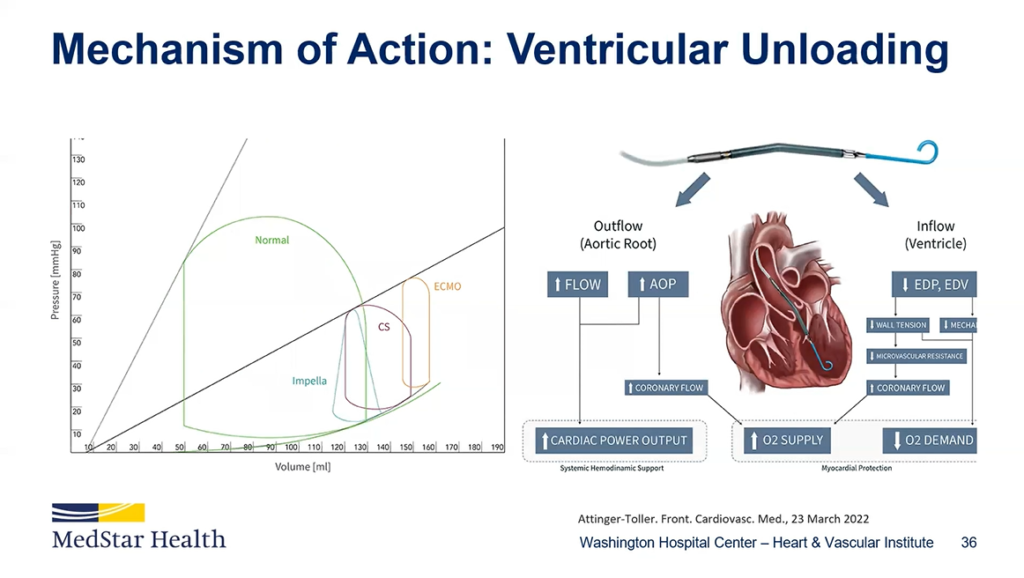
- Suction events – Changes in venous return, high pump speeds that cause increased LV unloading, & RV failure/increased pulmonary afterload
Two classifications:
- Primary Arrhythmia – caused by re-entry circuits or intrinsic to the heart’s own electrical system
- Secondary Arrhythmia – caused by a mechanical problem (usually under filled LV) causing the septum or free-wall that gets “sucked” into inflow cannula causing an arrhythmia
Interventions/Management
- Rule #1, don’t worry – they have an LVAD. Now here are some things you should worry about…
- Volume repletion
- Start with a 500cc fluid bolus as secondary causes of arrhythmias are common and can be easily fixed.
- May repeat bolus if MAP improves or patient clinically responds
- Adjust the VAD settings – done with the help of VAD team/engineers
- Discuss reducing the VAD’s pump speed in allow more time for the LV to fill
- Antiarrhythmic drug therapy
- First Line:
- Amiodarone – give it early and often
- Beta-blocker – most often metoprolol
- Second line: Sotolol, lidocaine, or mexiletine may also be given as an in-patient for refractory ventricular tachycardia.
- First Line:
- Refractory Ventricular arrhythmia management: Salvage treatments for patients with refractory VT include ablation therapy or implantation of RVAD. Electrical cardioversion in unstable patients has been described, but generally not used.
References
- Pedrotty DM, Rame JE, Margulies KB. Management of ventricular arrhythmias in patients with ventricular assist devices. Curr Opin Cardiol. 2013;28(3):360-8.
- Boyle A. Arrhythmias in patients with ventricular assist devices. Curr Opin Cardiol. 2012;27(1):13-8.
- Pratt AK, Shah NS, Boyce SW. Left ventricular assist device management in the ICU. Crit Care Med. 2014;42(1):158-68.
[/tab][/tabs]
[author title=”About the Author”]