[tab_nav type=”two-up”][tab_nav_item title=”Clinical Case” active=”true”][tab_nav_item title=”Answer” active=””][/tab_nav][tabs][tab active=”true”]
You receive a call from the neurosurgery intern who is frantic! He states that he is in desperate need of your help. Mr. DU is a 54 yo M who presented from home with “weak” legs and difficulty walking. The intern is panicking because he thinks the patient might have cauda equina syndrome, but it is hard to determine because the he has had saddle anesthesia and incontinence for many years stemming from a case of Fournier gangrene. Also, with his history of DM, HLD, and HTN many of his symptoms could also be vascular disease. A lumbar CT is negative and you agree to the mandatory neuro-checks and admit him to the unit. The initial neuro exam shows an underwhelming amount of weakness with ambulation.
The next morning you go over the MRI and find only a strange lesion in the thoracic spine:
When you freeze the image you see something suspicious in the region of T8-T9…
A re-examination shows increased weakness to the lower extremities as well as significant pain over the lower thoracic region. You go to the eMAR to write the order for empiric antibiotics and you see a peculiar test ordered by the neurosurgery intern:
QuantiFERON®-TB Gold: Positive
When asked, he states that the pt was recently incarcerated and he remembers that inmates get Tb (it was on step 2)
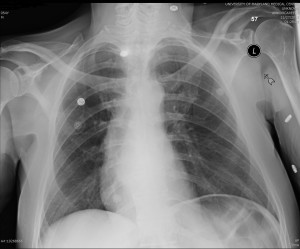
A frantic recheck of his CXR shows:
A million questions enter your head: Do you start isolation? What anti-tuberculosis medications do you need? how sensitive is QuantiFERON®-TB Gold?
The big question still looms: What you are you going to do?
[/tab][tab]
Background:
- Tuberculosis (Tb) of the spine (Pott’s disease) accounts for about 2% of all cases of Tb and 10% of extrapulmonary Tb
- Regions affected: lower thoracic spine (40-50%) > lumbar spine (35-45%) > cervical spine (10%)
- Typically involves 2 adjacent vertebral bodies with anterior wedging (due to disproportionate destruction of the anterior aspects of the vertebral bodies) and narrowing of the intervertebral disk space
- Pts will often experience months of spinal or radicular back pain before presentation
- Only 67% will have pulmonary Tb (the only Tb disease requiring drop-let isolation)
Physical Exam Findings:
- Localized Tenderness is #1 finding on exam and is non-specific
- Muscle spasms and decreased ROM are also common
- Thoracic kyphosis is the most common deformity found
- Typical Tb symptoms: fever, wt loss, night sweats, and malaise are typically not as apparent
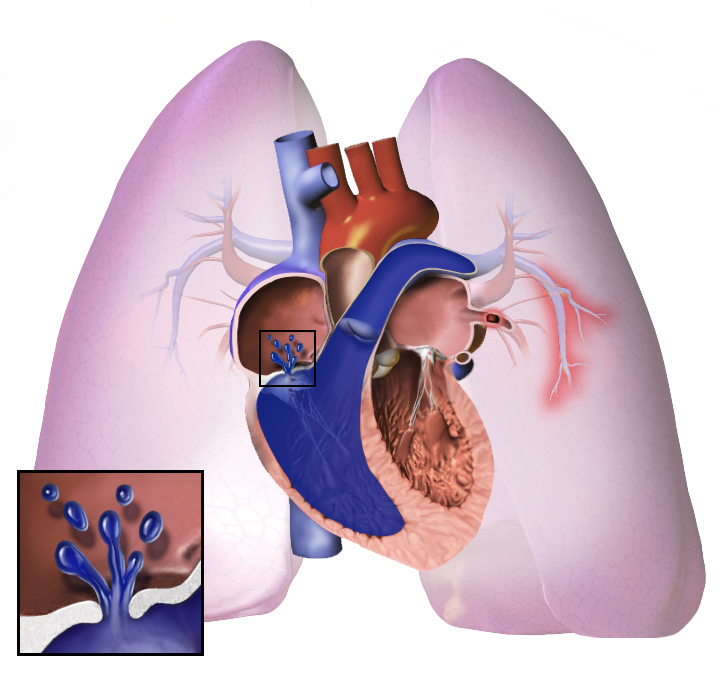
- Neurological deficits are a hallmark (50% of cases) and require emergency management
- Nerve root pain
- Paresis
- Sensory dysfunction
- Paraplegia
- Cauda equina syndrome
Testing for Pott’s Disease:
- PPD: positive in 84-95% of pts (without HIV coinfection)
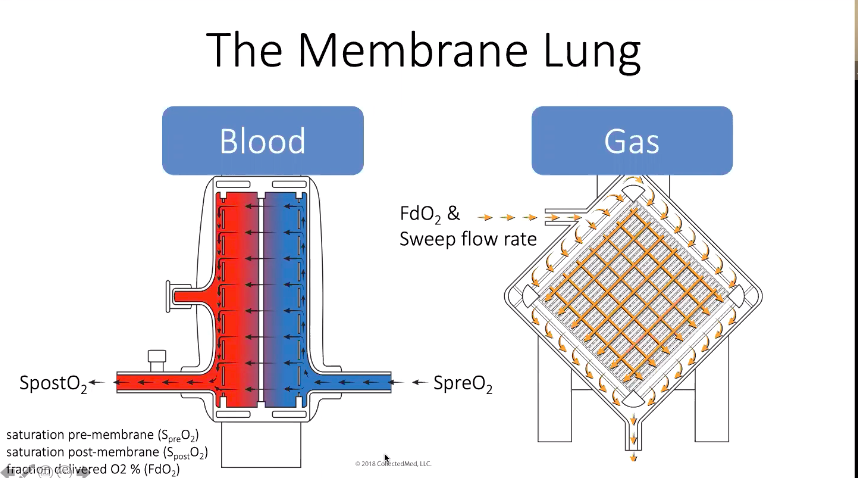
- PCR and immunological tests (QuantiFERON®-TB Gold): sensitivity: 84% and specificity: 95%
- Microbiological sampling: Gold standard is surgical biopsy (takes 6 weeks to grow!) as CT guided percutaneous samples are only positive in 50% of patients with active disease
- Xray findings: rarefaction of the vertebral end plates, loss of disk height, osseous destruction, new-bone formation and soft-tissue absces (at least one seen in 99% of patients)
- CT scan shows bone destruction: fragmentary in 47%; osteolytic in 34%, localized and sclerotic in 10%, and subperiosteal in 30% cases (see changes sooner then Xray)
- Bone scan: no specific changes noted; can be a hot or a cold spot (avascular disease)
- MRI: more sensitive than x-ray and more specific than CT
- Specific findings: Abscess formation+ granulation tissue adjacent to the vertebral body
Treatment
- 82-95% of pts respond well to medical therapy
- Intensive phase (2 months)
- RIPE therapy: Rifampicin, Isoniazid, Pyrazinamide, Ethambutol
- Can substitute in Streptomycin for Ethambutol (based on local patterns) for RIPS
- Remember pyridoxine when using Isoniazid (prevent peripheral neuropathy)
- Continuation phase:
- Isoniazid and Rifampicin
- 4 months minimum, but often needed for 12-24 months
- Goal: radiological or pathological evidence of regression of disease
References
- Garg RK, Somvanshi DS. Spinal tuberculosis: A review. J Spinal Cord Med. 2011 September; 34(5): 440–454.
- Turgut M. Spinal tuberculosis (Pott’s disease): its clinical presentation,
surgical management, and outcome. A survey study on 694 patients. Neurosurg Rev (2001) 24:8–13. - Pieschel D & Satterley C. Pott’s Disease. Physio-pedia.com
[/tab][/tabs]