This week, Dr. Bryan Hayes – Clinical Pharmacologist and expert in Toxicology gives an amazing talk highlighting 10 of his top tips for antimicrobial use in the emergency department & for the critically ill patient. This is probably one of the most clinically useful lectures I’ve listened to in a long time. Bryan has actually started his own campaign to make sure we are all using Vanc right in 2014 – he even made it a New Years Resolution of his own (Check out his post on Academic Life in EM)
Podcast: Play in new window | Download
Subscribe: Apple Podcasts | RSS
Pearls
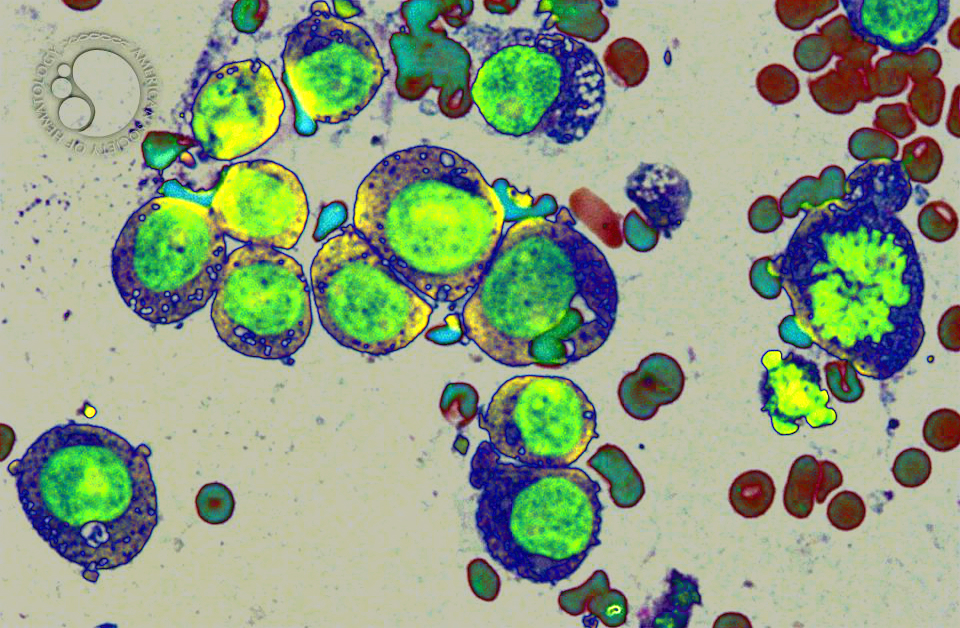
- How to correctly give a dose of vancomycin
- Dose: 15-20 mg/kg every 8-12 hours in patients with normal renal function, MAX: 2 grams
- Consider an even higher loading dose In seriously ill patients (e.g. sepsis, meningitis, infective endocarditis) with suspected MRSA infection: 25-30 mg/kg — again, MAX 2 grams (ISDA recommendation).
- Weight based dosing by using actual body weight
- In adults, we round to the nearest 250 mg increment (to help out your friendly pharmacist)
- In the critically ill obese patient, aminoglycosides should be dosed by adjusted body-weight
- ABW = Ideal BW + 0.4*(Actual BW – Ideal BW)
- A Penicillin allergy is NOT a contraindication to cephalosporin use!
- 3rd, 4th, & 5th Generation cephalosporins can be safely given to PCN allergic patients.
- Avoid keflex, cefaclor, cefadroxil, cefprozil as their beta lactam side chain is similar to PCN.
- Carbapenems are also safe in PCN allergic patients
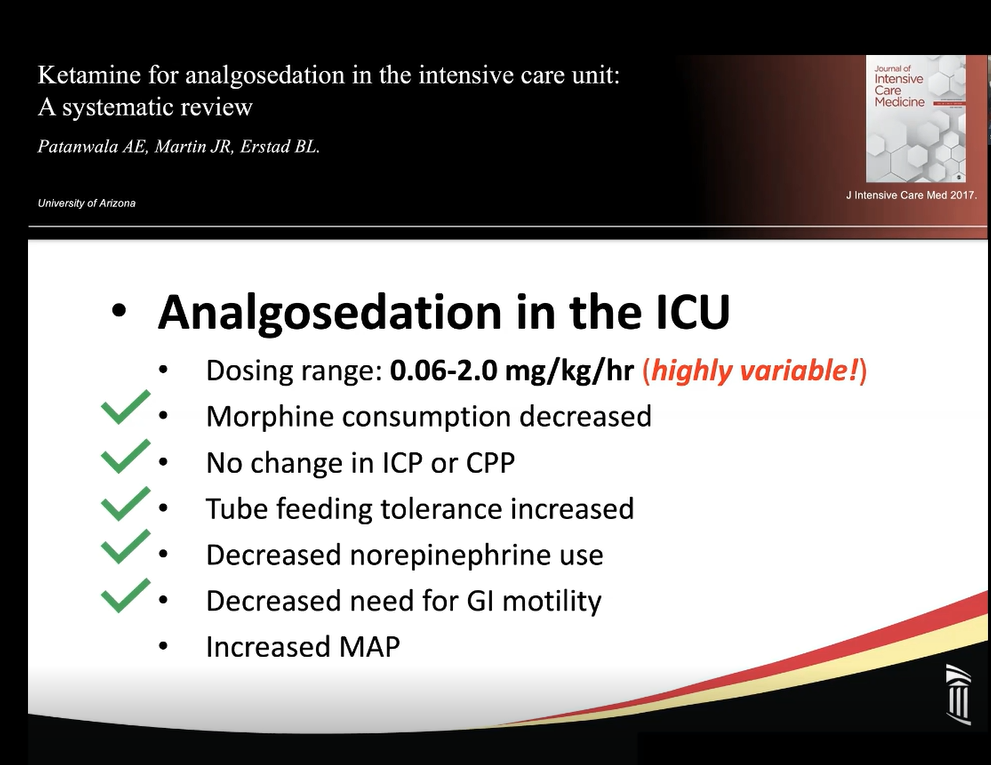
- HCAP “double coverage” should include only 1 beta-lactam antimicrobial, the 2nd agent should have a different mechanism of action (i.e. fluoroquinolone, etc.)
- Don’t forget the atypical coverage in HCAP patients! Send the urine legionella antigen.
- CAP patients admitted to the ICU should not be treated with a fluoroquinolone alone. Add the beta-lactam.
Thanks Bryan – we’ll make sure to get it right in 2014.
References
- Ryback M, et al. Therapeutic monitoring of vancomycin in adult patients: a consensus review of the American Society of Health-System Pharmacists, the Infectious Diseases Society of America, and the Society of Infectious Diseases Pharmacists. Am J Health Syst Pharm2009;66(1):82-98.
- Rosini JM, et al. Prescribing habits of vancomycin in the emergency department: are we dosing appropriately? J Emerg Med 2013;44(5):979-84.
- Liu C, et al. Clinical practice guidelines by the Infectious Diseases Society of America for the treatment of methicillin-resistant Staphylococcus aureus infections in adults and children.Clin Infect Dis 2011;52(3):e18-55.
- Fuller BM, et al. Emergency department vancomycin use: dosing practices and associated outcomes. J Emerg Med 2013;44(5):910-8.
- Frankel KC, et al. Computerized provider order entry improves compliance of vancomycin dosing guidelines in the emergency department. Am J Emerg Med 2013;31(12):1715-6.
- Campagna JD, Bond MC, Schabelman E, Hayes BD. The use of cephalosporins in penicillin-allergic patients: a literature review. J Emerg Med. 2012;42(5):612-20.