Today we are fortunate to have Dr. Ashutosh (Ash) Sachdeva, director of the University of Maryland Interventional Pulmonology Service and all around bronchoscopic wizard, to speak to us on his passion: how to save a failing airway. Over the next 60 minutes, Dr. Sachdeva will walk you through three procedures he feels that everyone staffing an ICU needs to know how to perform in their sleep. He may even toss in a few bronchoscopic secrets along the way.
Podcast: Play in new window | Download
Subscribe: Apple Podcasts | RSS
1) Cricothyroidotomy
- Simple technique in the right hands; however: need prior experience with technique before grabbing the scalpel (often takes 5 simulated attempts to be comfortable)
- Indications: can’t intubate/can’t ventilate (for a multitude of reasons), loss of upper airway landmarks (edema, facial/nasal injuries)
- Contraindications: overlying infection, tracheal injury, obscuring of landmarks (mass), age <12
- Adverse effects (based on prior studies): voice change (50%), tracheal stenosis (2%)
- Cheap kit: scalpel, bougie, 4-6 sz ETT and steady hands, though Seldinger-based kits are available
2) Percutaneous tracheostomy
- Advantages: short procedure, smaller incision needed, done at bedside (though OR can be used), lower VAP and lower LOS
- Disadvantages: requires bronchoscopic guidance (can injure bronchoscope), need advanced airway training
- Seldinger kits are available for ease of placement, though there is still need to visualize with bronchoscopy throughout the entire procedure (need 2 trained operators)
- Complications: puncture of posterior wall (by far most worrisome) & occlusion of trach with posterior wall tissue (due to inflammatory state)
3) Hemoptysis
- Actual definition varies: from 200 cc/hr of bleeding (healthy lung) to as low as 50 cc/hr (chronic respiratory failure) OR >2 episodes of moderate hemoptysis (~30cc) in 24 hours
- Cause: 90% from bronchial circulation (though non-bronchial sources can be more severe)
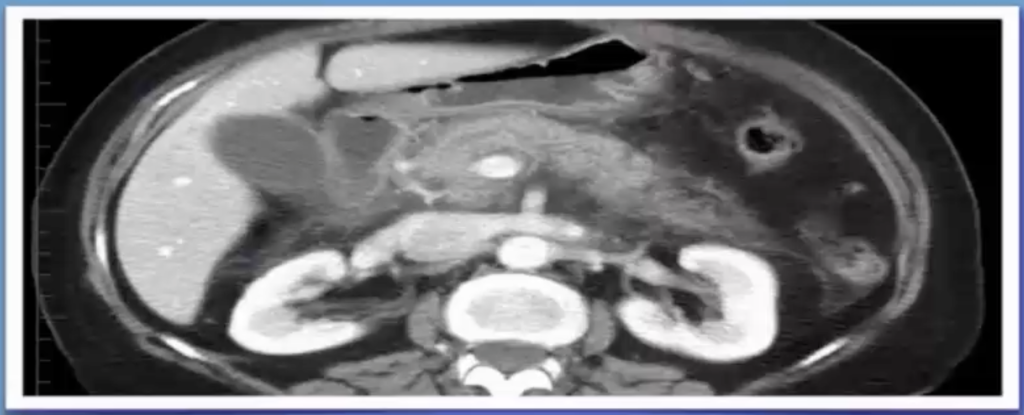
- CT scan with angio is gold standard; CXR will be diagnostic only 50% of the time
- Bronchoscopy: can help localize bleed and tamponade (bronchial blocker) to salvage healthy lung
**Special Note: Tracheo-innominate artery fistula– due high riding innominate or low riding trach (below 4th tracheal ring– most common cause); appears by week 3-4, often preceded by sentinel bleed!**
References
- Ernst A, Feller-Kopman D, Becker HD, and Mehta AC “Central Airway Obstruction”, American Journal of Respiratory and Critical Care Medicine. 2004;169(12):1278-1297.
- Theron J, Diacon AH, and Bolliger CT. Chapter 7. Management of massive haemoptysis. European Respiratory Monograph 36: Respiratory Emergencies. 2006;36:95-107.
- De Leyn P, Bedert L, Delcroix M, Depuydt P, Lauwers G, Sokolov Y, Van Meerhaeghe A, and Van Schil P. Tracheotomy: clinical review and guidelines. Eur J Cardiothorac Surg. 2007;32:412-421.
- Sachdeva A, Shepherd RW, Lee HJ. Thoracentesis and thoracic ultrasound: state of the art in 2013. Clin Chest Med. 2013 Mar;34(1):1-9.