[tab_nav type=”two-up”][tab_nav_item title=”Clinical Case” active=”true”][tab_nav_item title=”Answer” active=””][/tab_nav][tabs][tab active=”true”]
Since 1922, physicians have been using the long bones as a “non-collapsible vein” for fast and reliant resuscitation. Although first targeted to war-time efforts, the 1980s brought the use of intraosseous (IO) access into EMS and hospital protocols, often used when alternative means of access have failed. However, in the austere world where there is a limitation in both resources and training, the IO may be the only means available for central access.
This is a video of Dr. L. Nathalie Colas placing the first IO line used in St Luke’s Hospital, Port-au-Prince, Haiti for central access in an obtunded patient (finger stick of 22 mg/dl and hypothermic) with presumed sepsis:
When I presented this new use to my program here in Maryland many questions arose:
How reliable is this access? How long can we use it? Are there any drugs we cannot infuse? Are there any complications one must watch out for?……….
[/tab]
[tab] Answer:
Intraosseous Access
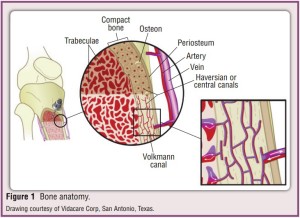
Fluids introduced into the trabeculae (medullary canal) → central circulation Day MW. Critical Care Nursing 2011
- Benefits:
- Access in <30 seconds with minimal training (avg 4.5-120 seconds)
- Success rates: 75%-100%
- Similar onset of action and drug levels when compared to IV (vasopressors!)
- Common labs (ABG, metabolic panels, CBC, drug lvls, etc) are comparable to peripheral values
- Caveat: electrolytes and acid/base status not accurate s/p multiple infusions/drug administrations
- Indications:
- Critical ill patients (any age) where access is required
- Useful for crashing obese pts, seizing pts, or pts with severe edema (access nightmares)
- Critical ill patients (any age) where access is required
- Contraindications:
- Long bone fractures
- Vascular injury
- Overlying skin infection/burn
- Any iatrogenic fracture risk: osteogenesis imperfecta or osteoporosis
- Any site of previous IO insertion (fluids may extravasate from previous sites)
- Complications:
- Inadequate access: displaced needle or posterior cortex puncture
- 0.8%: extravasion of materials → compartment syndrome
- 0.6%: osteomyelitis (associated with prolonged use > 24 hours)
- 0.1%: subcutaneous abscess
- Sternal access risks: PTX, cardiac injury, injury to great vessels, and death (rare but significant)
- Equipment:
- Standard universal precautions + antiseptic solution
- 1–2 mL of a 1% or 2% lidocaine solution without epinephrine (site infiltration for awake pts)
- One of 3 means of access:
- Manual needles
- needle with a central trocar to penetrate into the marrow cavity
- Pros: Simple to use, lightweight, and reusable (in the same pt)
- Cons: protrude above skin (~2cm)= less stable + easy to dislodge, need significant insertion force (prone to bending, breaking)
- Impact driven needles
- Two types available: FAST1 system (sternal only) and Bone Injection Gun (humerus, tibia)
- Pros: very secure, very fast (<10s), success rate can approach 100% (with training)
- Cons: heavy, single use (so any miss is a missed opportunity), sternal use can limit CPR and use of a c-collar
- Power driven needles (ie: EZ-IO)
- 3 sizes available (depending on age of patient and site desired)
- Pros: easy to use, simple to teach, very fast (<10s), driver is reusable (~1000 times), little pain with placement (equated to an 18G needle, even without lidocaine)
- Cons: very expensive (large initial investment for drivers + needles), heavy and bulky system to carry
- Manual needles
- Sites of Insertion (per industry guidelines) is any thin cortex bony site:
- Pediatric:
- Sites: proximal tibia, distal femur, humerus, distal ulna, distal tibia, sternum (>12yo)
- Adults:
- Preferred: sternum, proximal tibial plateau, proximal humeral head, medial malleolus
- Other options: clavicle, distal radius or ulna, ilium
- Last resort is bones without a medullary cavity: calcaneus and radial styloid
- Simple guidelines:
- Code: proximal tibia (far away from chest compression, thin overlying skin and thin cortical bone)
- Battlefield: sternum (reliable access with risk of extremity injuries)
- Fastest: sternum = proximal humerus (but humeral is more practical in hospitalized patients)
- Pediatric:
Luck RP, et al. J Emerg Med 2010
- Tips: (courtesy Dr. Larry Mellick)
- Assess needle length BEFORE placement; will need 5mm of needle to enter bone (or one black line)
- Push needle through skin FIRST, then start drilling (allows better sizing and avoids twisting skin)
- STABILIZE extremity
- Steady DOWNWARD force only, any axillary force can bend/break needle or widen hole and allow extravasion
- FLUSH the needle to maximize flow through the bony cortex
- Replacement as central access?
- Although IOs have been left in for up to 96 hours, the recommended time is up to 24hrs (increased risk of infection)
- In an environment, such as Haiti, there are no other options for central access
- Further research is required before longer use can be recommended outside of austere environments
References
- Luck RP, Haines C, Mull CC. Intraosseous access. J Emerg Med. 2010 Oct;39(4):468-75.
- Day MW. Intraosseous devices for intravascular access in adult trauma patients. Crit Care Nurse. 2011 Apr;31(2):76-89.
- Weiser G, Hoffmann Y, Galbraith R, Shavit I. Current advances in intraosseous infusion – a systematic review. Resuscitation. 2012 Jan;83(1):20-6.
[/tab]
[/tabs]