Dr Henry Masur is a clinical expert in HIV from the National Institute of Health (NIH) who has published over > 300 peer reviewed publications related to infections and HIV. We were tremendously lucky to have hime come up to Baltimore and give a really nice review on the history of HIV as well as some major pearls and pitfalls to consider the next time your managing a patient with HIV patient in your ICU. You think you may know how to manage the sick patient with the classic opportunistic infection – but what about the trauma patient with HIV? How about that HIV patient who just had an MI? You can really make some big mistakes if you go at it alone.
Podcast: Play in new window | Download
Subscribe: Apple Podcasts | RSS
- We may not be making as much progress as we think in HIV care
- HOPS Study – while optimistic, is based on a sample of patients who are compliant with out-patient care.
- NHDS – based on discharge summaries, shows we may not be doing that well with treating HIV and preventing OI’s.
- For any HIV patient in the ICU – it should automatically trigger you to give your friendly Infectious Disease consultant a call. Medications are complex, have lots of interactions, and shouldn’t be managed alone.
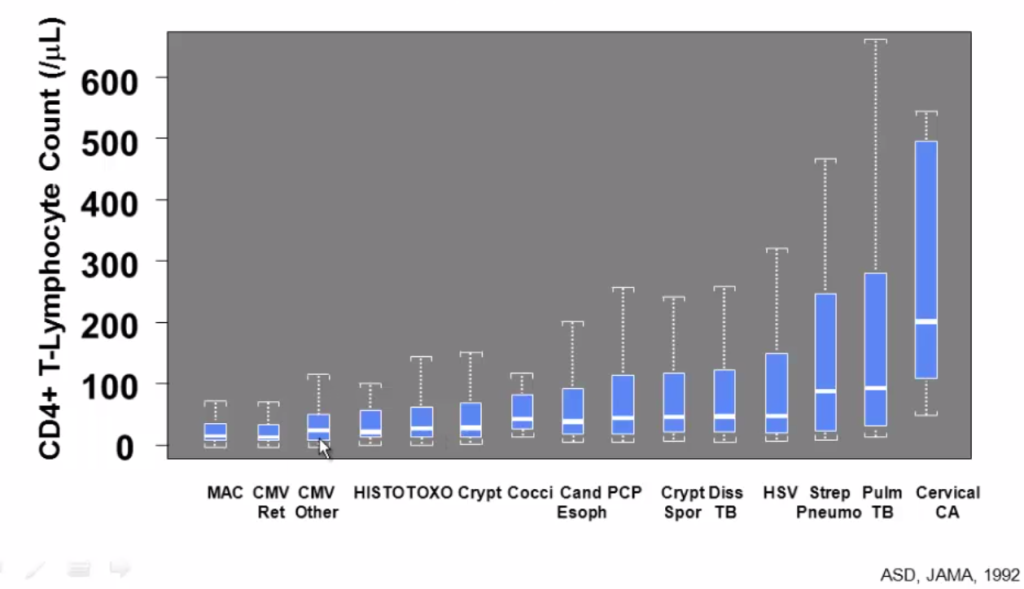
- Pearl: When do opportunistic infections occur? The CD4 cut off may not be what you were actually taught!!
- HIV issues to be aware of:
- Absorption issues: Resistance to subtherapeutic levels (nearly all meds are oral) of HIV meds can happen within DAYS. Once a resistance is established, they will have forever lost the ability to take that antiretroviral ever again.
- Toxicities:
- Abacavir: Distributive shock (Sepsis mimic), desquamating rash, hypersensitivity syndrome.
- Dapsone: Methemoglobinemia
- Fluconazole, bactrim, INH, rifampin: hepatitis
- Drug Interactions: Often interact with many drugs used in the ICU
- Ritonavir, Rifampin – lots of interractions
- Immune Reconstitution Inflammatory Syndrome (IRIS)
- Important to ask your HIV patient when they started their anti-retroviral therapy (ARVs) – classic time line for IRIS is days to weeks.
- HIV & Pneumonia – Pneumococcus, Hemophilus, PCP, Tuberculosis, & Atypicals/Viral infections are the most common causes. Don’t for get about S. Aureus either!
- Refractory PCP: Clindaprimaquine is just as good as IV Pentamadine. Atovaquone is a BAD CHOICE due to the fact that it’s an oral drug and has the potential for erratic absorption and subtherapeutic levels.
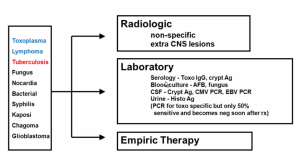
- HIV + CNS Mass lesions: CD4 < 100 – think Toxoplasma or Lymphoma. If the CD4 > 100, it’s not Toxo, think lympoma, Tb, or something else.
References
- Fauci AS, Folkers GK. Toward an AIDS-free generation. JAMA. 2012;308(4):343-4.
- Steinbrook R. HIV/AIDS in 1990 and 2012: from San Francisco to Washington, DC. JAMA. 2012;308(4):345-6.