Today we are fortunate to have Avelino Verceles, Associate Professor of Critical Care and Pulmonary Medicine here at the University of Maryland as well as acting director and architect of one of the most successful ventilator weaning programs in the Northeast. Over the next hour, Dr. Verceles will explore the devastating complications suffered by the “survivors of critical illness” and explain the way rehab can save more then just muscle mass…..
Podcast: Play in new window | Download
Subscribe: Apple Podcasts | RSS
Pearls:
Background
- 90% of patients who suffer an acute critical illness will quickly recover or die
- 10% of patients will be classified as “survivors of critical illness”
- Prolonged mechanical ventilation, tracheostomy, deconditioned, multiple comorbidities
- Consume 40% of ALL ICU resources during their ACUTE stay (or $20 billion!!)
- 40% of all ICU admissions are mechanically ventilated for a mean time of 2-4 days
- 5-20% will remain intubated >7 days
- At 21 days the patient is qualified as “chronically critical ill”
- 75% of the chronically critical ill are over the age of 50yo
- FACT: 1/2 of all patients admitted to the ICU >65yo will eventually be qualified as chronically critical ill
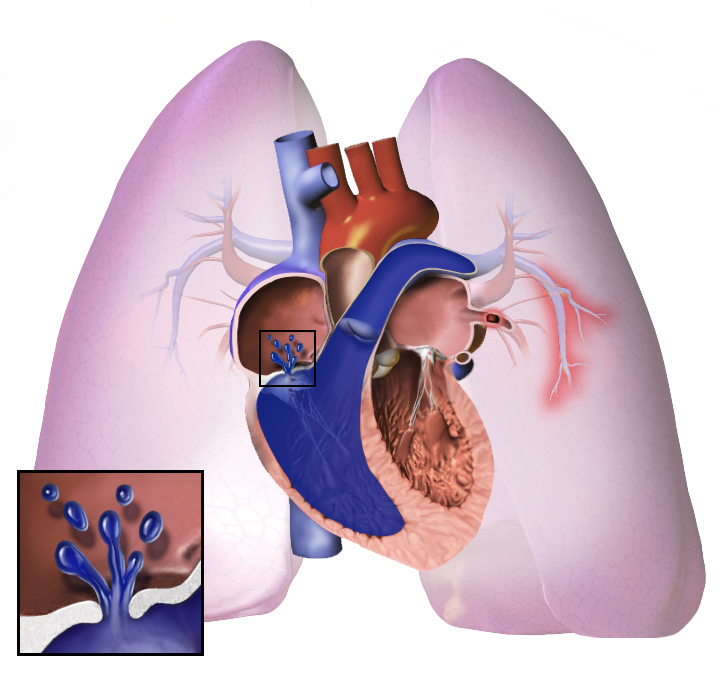
- Complications of prolonged mechanical ventilation:
- Delerium, PTSD, ↓ cognitive function, ↓ quality of life
- Malnutrition: under- or over-feeding
- Sarcopenia, muscle atrophy, deconditioning, loss of function → decreased mobility
- Critical illness neuromyopathy
- 50% of patients admitted with sepsis and/or multiorgan failure will suffer severe myopathy
- 90% of patients will have persistent abnormalities at 5 years
- 50% of ICU survivors have severe difficulties with ADLs at 1 yr
- 50% of patients admitted with sepsis and/or multiorgan failure will suffer severe myopathy
Weaning
- >50% of chronically critically ill patients can be weaned by 1 yr of discharge
- Ventilator associated pneumonia (VAP) effects 40% of pts ventilated >7 day
- There is a cumulative 1% risk of developing a VAP every day the patient is ventilated
- #1 way to wean off the vent is via respiratory therapist driven protocols (30-53% weaning rate!)
- Rapid Shallow Breathing Index (RSBI): RR/VT
- Spontaneous Breathing Trial (SBT)
- Out of bed to chair (OOBTC)
- Pulmonary toileting, Percussion therapy
- When to start weaning:
- Acute problem has resolved
- Hemodynamically stabilized
- Appropriate mental status
- Airway intact
- SBT is tolerated
- Process of performing a SBT:
- Short (30 mins) vs long (120 mins): equal extubation, intubation, and mortality rates
- Trach collar trials have better outcomes than decremental pressure support trials (Jubran A. JAMA 2013)
Nutrition
- 43% of critically ill are malnourished (under- or overfed) leading to poor outcomes
- ↑ proteolysis, ↑ cellular use of protein, ↓ creation of albumin (all efforts switched to creating acute phase reactants)
- ↑ risk of infections, ↑ ICU LOS, ↑ mortality, ↓ ventialtor free days
- Kwashiorkor malnutrtion: ↓ lean tissue mass, anasarca, hypo-oncotic state
- Refeeding syndrome: reintroduce a large nutritional load → insulin surge → electrolyte abnormalities (↓PO4, ↓Mg, ↓K)
- Avoid with early enteral nutrition with “permissive underfeeding” for the first 2 days
Early Ambulation
- Lose 1.5kg/day of skeletal muscle (~50% of muscle mass gone in 2 weeks!)
- ↑ rate with multiorgan failure or severe sepsis
- Avoid with the use of early ambulation and ↑ ROM exercises
- A properly tailored regime will maximize muscle strength (functional), muscle endurance, and aerobic exercises
- ↑ functional status at discharge, ↓ delerium, ↑ ventilator free days, ↓ costs
References
- Jubran A, Grant BJ, Duffner LA, Collins EG, Lanuza DM, Hoffman LA, Tobin MJ. Effect of pressure support vs unassisted breathing through a tracheostomy collar on weaning duration in patients requiring prolonged mechanical ventilation: a randomized trial. JAMA 2013 Feb 20;309(7):671-7.
- Scheinhorn DJ, Hassenpflug MS, Votto JJ, Chao DC, Epstein SK, Doig GS, Knight EB, Petrak RA; Ventilation Outcomes Study Group. Post-ICU mechanical ventilation at 23 long-term care hospitals: a multicenter outcomes study. Chest 2007 Jan;131(1):85-93.
- Puthucheary ZA, Rawal J, McPhail M, Connolly B, Ratnayake G, Chan P, Hopkinson NS, Phadke R, Dew T, Sidhu PS, Velloso C, Seymour J, Agley CC, Selby A, Limb M, Edwards LM, Smith K, Rowlerson A, Rennie MJ, Moxham J, Harridge SD, Hart N, Montgomery HE. Acute skeletal muscle wasting in critical illness. JAMA 2013 Oct 16;310(15):1591-600.
- Schulman RC, Mechanick JI. Metabolic and nutrition support in the chronic critical illness syndrome. Respir Care 2012 Jun;57(6):958-77; discussion 977-8.