The Case:
- 64 yo M veteran smoker w PMH severe COPD on 4L O2 by NC, pAfib on AC, admitted in December for progressive dyspnea over weeks, found to have a bronchus intermedius obstruction due to extrinsic compression from a NSCLC mass near the right hilum.
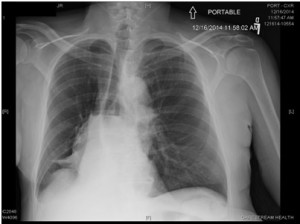
Portable CXR on admission
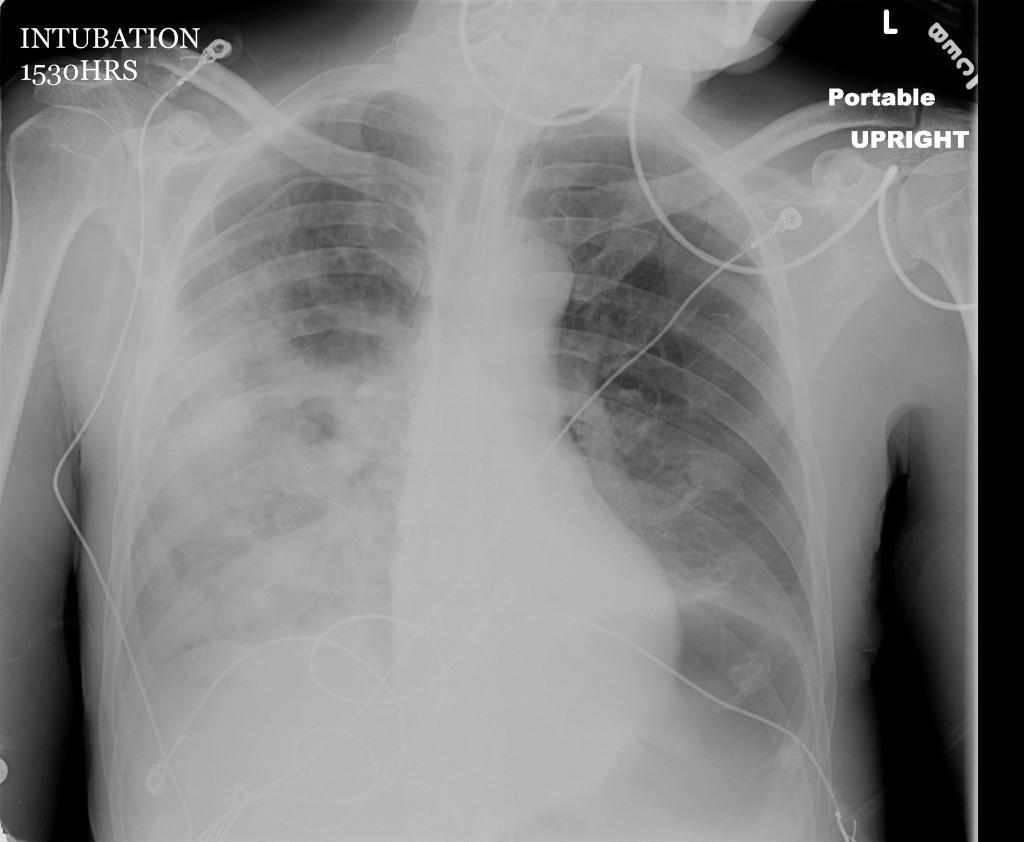
Portable CXR 3 days later
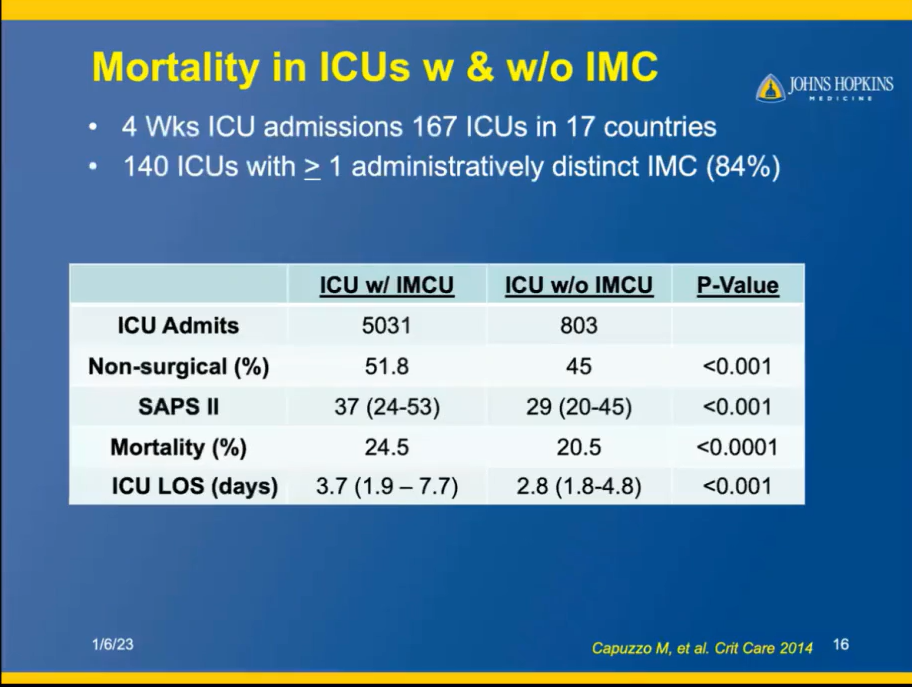
- Basic Statistics on Morbidity & Mortality in NSCLC
- 5 yr Survival NSCLC (w Rx):
- Stage I: 60-80%
- Stage II: 40-50%
- Stage III: 10-20%
- Stage IV: <<10%
- 40-85% of NSCLC patients will have symptoms related to the primary tumor.
- Cough, dyspnea, wheeze, hemoptysis
- QoL is influenced by:
- Tumor itself
- Metastases
- Treatment
- Paraneoplastic syndromes
- 5 yr Survival NSCLC (w Rx):
- Indications for airway stenting are:
- Extrinsic stenosis of central airways with or without intraluminal components due to malignant or benign disorders
- Complex, inoperable tracheobronchial strictures
- Tracheobronchial malacia
- Palliation of recurrent intraluminal tumor growth
- Central airway fistulae (esophagus, mediastinum, pleura)
- Contraindications
- Nonviable lung is present beyond the obstruction
- Extrinsic compression of an airway by a vessel
- Stent related complications
- Displacement
- Mucus impaction
- Granuloma formation at stent ends
- Re-obstruction by tumor
- Halitosis
- Infection
- Perforation of airway walls
- Hemoptysis
- Pain
- Cough
- Fire (during laser resection)
NOTE: No prospective, randomized trials exist on the utility of palliative stenting for proximal airways obstruction for obvious ethical reasons. The following conclusions were drawn from single-center prospective cohort / observational studies published in the literature about their centers’ experience with these patients and their centers’ available interventions.
Conclusions
- Interventional Pulmonology procedures (such as stenting) should be considered for palliation of large airway obstruction in malignant disease
- Patients can anticipate an improvement in dyspnea and spirometric measures, but overall QoL is not as clear
- Complications are not rare, but most patients demonstrate overall benefit from intervention.
- With achieved airway patency, mortality approximates that of patients without previous obstruction. However, no center to date has evaluated the impact of large airway stenting versus not-stenting on mortality from malignant endotracheal or endobronchial obstruction. One can imagine the challenging ethical issues regarding this.
References
- Bollinger et al. ERS/ATS statement on interventional pulmonology. Eur Respir J 2002; 19: 356-373
- Chhajed PN, Baty F, Pless M, et al. Outcome of treated advance non-small cell lung cancer with and without airway obstruction. Chest 2006;130:1803–7.
- Ferrell et al. Palliative Care in Lung Cancer. Surg Clin North Am. 2011 April ; 91(2): 403–ix.
- Amjadi et al. Impact of Interventional Bronchoscopy on Quality of Life in Malignant Airway Obstruction. Respiration 2008; 76: 421-428.