Welcome to a momentous occasion for MCCP. Today we have Dr. Rahul Nanchal, the co-Chair of both the SCCM and ESICM task force on hepatic failure in the ICU; making him one of the world’s foremost experts in the field of liver failure! Dr. Nanchal visits from the Medical College of Wisconsin where he has both an Associate Professorship in Pulmonary and Critical Care Medicine and acts as the medical ICU director. Dr. Nanchal is also well published in the field and is currently the principle investigator for the novel use of extracorporeal liver assist devices in acute decompensated alcohol induced liver failure. We are very fortunate that even with his busy schedule he was able to stay in Baltimore long enough to impart his many years of knowledge and wisdom in one amazing lecture. If you ever plan to correctly treat the cirrhotic in your ICU you CANNOT MISS this talk!
Podcast: Play in new window | Download
Subscribe: Apple Podcasts | RSS
#1 Principle: Vasodilated State
- ↑ portal venous pressure → ↑ splanchnic vasodilation → ↑ splanchnic flow → ↑ splanchnic pressure → ↑ splanchnic shunts → ↑ portal venous pressure…. and repeat to decompensation….
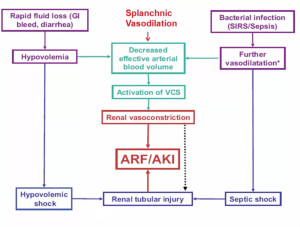
#2 Principle: Complicated Hemodynamic State
- Significantly decreased effective blood volume
- Any additional loss of vascular tone/volume (sepsis, GIB, overdiuresis) leads to SIGNIFICANT organ dysfunction!
- Baseline MAP is decreased
- difficult to define sepsis, shock, hypotension
- Abnormal lactic acid and ScVO2 values are the norm
- Cirrhotic cardiomyopathy with depressed systolic and diastolic function is common
- Adrenal insufficiency is nearly expected with significant liver dysfunction further complicating management
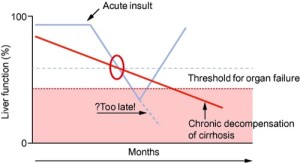
#3 Principle: You must recognize Acute decomposition of Chronic disease!
- An acute drop in baseline liver function should start the investigation for infection (#1 cause!)
- If caught early and treated aggressively there is reversibility (but never to baseline!)
Jalan, et al. Journal of Hepatology 2012 57, 1336-1348
- Diagnosis
- Worsened coagulopathy (INR >1.5)
- Encephalopathy (NO cerebral edema!)
- Pre-existing liver disease
- Illness duration < 26 weeks
- New organ failure (AKI is #1)
- Mortality at 3 months is 33% compared to 2% at baseline (source)
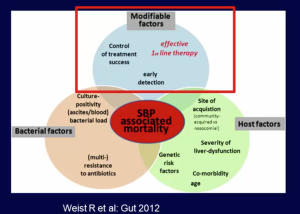
#4 Principle: Infections are the #1 cause of mortality
- UTI: #1 infectious cause of decompensation
- most nosocomial and preventable (catheter hygiene)
- SBP: Traditionally > 250 PMNs in ascites, however <250 PMNs diagnostic if gram positive is source!
- Hemorrhagic (>10k RBCs): subtract 1 PMN for each 250 RBCs
- Nosocomial SBP (>48 hours hospitalization) needs abx escalation as MDR bacteria is common
- C. diff: #1 infectious cause of mortality
- Antibiotic choice is important! (source)
- 1/4 of patients are placed on wrong initial antibiotic (8% never get proper abx!)
- Median time to abx: ~7.5 hours!
- Mortality >75% if incorrect abx chosen!
#5 Principle: Acute Kidney Injury is just the beginning
- AKI: most common extra hepatic injury and a major contributor to mortality
- Most commonly caused by infection (#1 SBP)
Garcia-tsao et al. Hepatology 2008; 48:2064
- Compromised platelet function and severely elevated anion gap metabolic acidosis are common
- Hepatic-Renal Syndrome is difficult to diagnose as creatinine and FENa are nearly impossible to interpret
- Often a diagnosis of exclusion
- Tx with vasoconstrictors (Terlipressin or Midodrine/Octreotide) + Albumin (volume effect + anti-oxidant)
- If RRT is needed > 6-8 weeks, hepato-renal transplantation may be only cure
- Mortality is 10x higher if renal function never recovers
#6 Principle: Recognize the early signs of GI disease states
- Varices: Size, Red Whale sign, and Child class B/C is predictive of bleeding
- Tx with RBC conservatively (unless hemorrhaging, keep hgb ~ 7.0)
- ALWAYS give abx! Prevent both SBP and re-bleed!
- Tx with vasopressors early (Vasopressin, Octreotide, Somatostatin)
- IAH: IAP >12 mmHg vs. ACS: IAP >20mmHg
- Regardless of the level, treat aggressively as both states can worsen AKI and increase mortality
- Ileus is common with lactulose, a better alternative for critically ill pts is PEG bowel prep (better outcomes)
#7 Principle: Pulmonary insults are VERY common
- Hepatopulmonary Syndrome (HPS)
- Vasodilators from hepatic circulation (NO) → pulmonary vasodilation → O2 diffusion impairment
- Hypoxemic w/o radiological changes
- Platypnea + Orthodeoxia (SOB and hypoxic when standing) due to preferential basilar vasodilation
- 10-32% prevalence
- RA PO2 <50 mmHg = Increased mortality
- Dx by TTE: look for late bubbles on study
- Reversible by liver transplant
- Portal Pulmonary HTN
- ↑ risk of acute RV failure with TIPS!!
- Will NOT reverse with liver transplant
- Hepatic Hydrothorax
- Diaphragmatic defect → Ascites in thoracic cavity
- Can get SBP of this fluid (same dx criteria)
- Tx with drain, TIPS, or Pleurex catheter
- Diaphragmatic defect → Ascites in thoracic cavity
- Jalan R, Gines P, Olson JC, Mookerjee RP, Moreau R, Garcia-Tsao G, Arroyo V, Kamath PS. Acute-on chronic liver failure. J Hepatol. 2012 Dec;57(6):1336-48. [PubMed Link]
- Romero-Gómez M, Montagnese S, Jalan R. Hepatic encephalopathy in patients with acute decompensation of cirrhosis and acute-on-chronic liver failure. J Hepatol. 2015 Feb;62(2):437-47. [PubMed Link]
- Wong F, Nadim MK, Kellum JA, Salerno F, Bellomo R, Gerbes A, Angeli P, Moreau R, Davenport A, Jalan R, Ronco C, Genyk Y, Arroyo V. Working Party proposal for a revised classification system of renal dysfunction in patients with cirrhosis. Gut. 2011 May;60(5):702-9. [PubMed Link]
- Bajaj JS, O’Leary JG, Reddy KR, Wong F, Olson JC, Subramanian RM, Brown G, Noble NA, Thacker LR, Kamath PS; NACSELD. Second infections independently increase mortality in hospitalized patients with cirrhosis: the North American consortium for the study of end-stage liver disease (NACSELD) experience. Hepatology. 2012 Dec;56(6):2328-35. [PubMed Link]