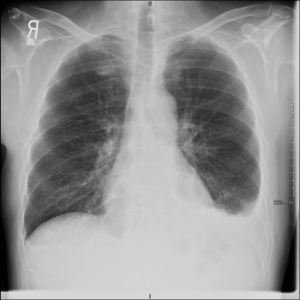
THE CASE: A 68 yo M w PMH recently diagnosed R arm fibromyxosarcoma with known metastatic disease to the lungs, s/p 1 cycle of Gemcitabine & Docetaxel, as well as prior L PTX 2 months prior to presentation presents with an asymptomatic pleural effusion on the L that is new by report. No infectious symptoms of any kind. Pulmonary was consulted after CXR revealed the effusion in the ED.
IMAGING:
LABS — Thoracentesis Results:
Glu: 126; LDH: 121 (Serum > 250); T Prot 1.7 (Serum 6.0)
Cell Count: RBC 0; WBC 2100 (82% EOS)
EOSINOPHILIC PLEURAL EFFUSION (EPE):
Definition: Pleural fluid in which differential cell count reveals > 10% Eos.
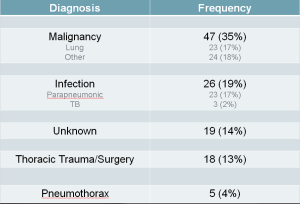
A brief history: First described by W. Harmsen in 1894, with first case described in the United States at Hopkin’s in 1916 (see references below). It wasn’t until the 1960s when a large case series written by Campbell & Webb that it really began to be looked at in earnest about the meaning of such a finding. Larger papers in the 1980s and 1990s (Kuhn et al, Rubins & Rubins, & Martinez-Garcia et al)described single center experiences with EPE and the ultimate diagnoses of these patients, all essentially concluding that no specific diagnostic category (malignant versus non-) or particular diagnosis (e.g. TB) was implied by the finding of EPE. In 2009, Krenke et al out of the University of Warsaw — published in ERJ — made the following observations based upon 2200 pleural effusion samples:
- Approximately 7% (n = 135) of all pleural effusions meet criteria for EPE
- EPE was twice as common in men than in women, despite overall effusions being present in a roughly 1:1 ratio.
- The underlying etiology for EPE was:
- Perhaps most interestingly, higher pleural eosinophil counts were less frequently associated with malignancy. In other words, pleural eos > 40% were less likely to be attributated to malignancy (Sn 85%, Sp 35%).
Case Wrap-Up: My patient tolerated his procedure well. His cytology was negative. I brought him back one week later and his effusion had not recurred. Ultimately this was probably related to his recent pneumothorax or his chemotherapy. This was discussed with his oncologist and decided that should it recur, steroids would be incorporated into his chemo cycle to minimize future recurrences.
CONCLUSION / Take-home Points:
- Eosinophilic Pleural Effusions (EPE) are present in 7-10% of all unilateral pleural effusions, and are defined as a pleural eosinophil count > 10% on cell diff.
- The present of an EPE is not indicative of any particular diagnostic category (malignancy vs non-) or particular diagnosis (such as TB, for example).
- Higher pleural eosinophil counts (esp. those > 40%) are less frequently associated with malignancy than lower cell counts (Sn 85%, Sp 35%).
- Certain drugs / chemotherapies (particularly the combination of Gemcitabine & Docetaxel in this patient) are frequently associated with pulmonary toxicity, of which new effusion is one of the potential complications. Steroids has been shown to mitigate this.
References:
- Light, Richard. Pleural Effusion. NEJM 2002. 346(25): 1971-77.
- Krenke et al. Incidence and aetiology of eosinophilic pleural effusion. Eur Respir J 2009; 34: 1111–1117.
- Rubins & Rubins. Etiology and Prognostic Significance of Eosinophilic Pleural Effusions. Chest 1996. 110: 1271-74.
- Martinez-Garcia et al. Diagnostic utility of eosinophils in the pleural fluid. Eur Res J. 1999. 15: 166-169.
- Kuhn et al. Probability of malignancy in pleural fluid eosinophilia. Chest 1989. 96: 992-94.
- BTS Pleural Disease Guideline 2010
- Charpidou et al. Therapy-induced Toxicity of the Lungs: An Overview. Anticancer Research. 2009. 29: 631-40.
- Bronstad et al. Effects of the taxanes paclitaxel and docetaxel on edema formation and interstitial fluid pressure. Am J Physiol Heart Circ Physiol 287: H963–H968, 2004