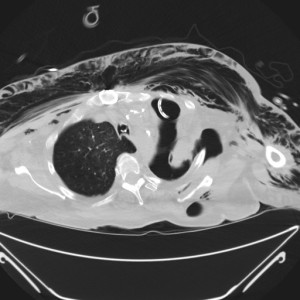
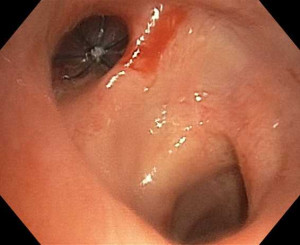
Imaging of a BPF:
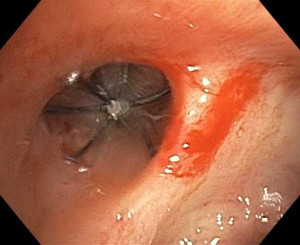
Bronchoscopic Closure:
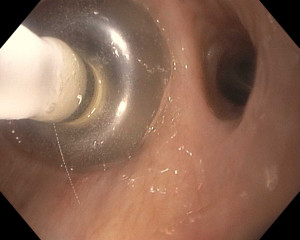
Visualization of defect:
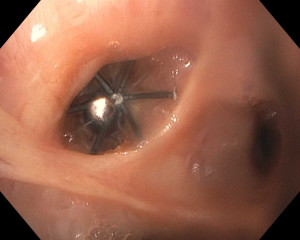
Balloon deployment and valve placement:
Bronchopleural Fistula (by Dr. Kami Hu)
Bronchopleural fistulae (BPF) are more than simply air leaks to be fixed with a chest tube. Albeit relatively rare, they carry a high morbidity and mortality, and knowledge regarding their management is important to facilitate healing and limit negative outcomes.
A brief review of physiology reminds us where the goalposts stand in terms of ventilator management, tube thoracostomy drainage, and the careful maintenance of a low transpulmonary pressure gradient that prevents flow through the fistula tract.
In healthy, intact lung, the transpulmonary pressure is the difference between alveolar pressure and intrapleural pressure:
Ttp = Palv – Pip
In a lung with BPF, there is a new transpulmonary pressure:
Ttp = Paw – Pip
Flow across the tract increases with lower BPF resistance (wider, shorter fistulae), increased airway pressures, and more negative intrapleural pressures.
Flow BPF α Airway Pressure (Paw) – Intrapleural Pressure (Pip) Resistance BPF
In our ventilated patients with BPF, our aim is to decrease the transpulmonary pressure gradient and keep airway pressures lower than the pressure required to overcome the resistance of the fistula. Minimize PEEP and tidal volumes, and limit positive inspiratory pressure by utilizing partial support modes when possible, decreasing respiratory rates, and increasing flow rates to decrease inspiratory time. These goals may not be achievable in all patients; acid-base abnormalities, ARDS, and chronic lung disease may require more than minimal settings. Other options for these patients include high frequency ventilation or independent lung ventilation (also called dual lung ventilation) and even ECMO.
With regards to chest tubes, two main considerations
- Ensure the tubes are sized appropriately. Just like the fistula, flow is increased with larger french size and shorter tubes have less resistance. Larger tubes may be required for high-flow air leaks and for appropriate drainage of infection.
- Avoid unnecessary suction. Increased suction results in more negative intrapleural pressure, increasing the transpulmonary gradient and thereby increasing flow through the fistula.
Methods of definitive treatment for persistent bronchopleural fistulae include the old mainstay, surgical intervention, but the various other interventions available via fiberoptic bronchoscopy (sealant application, closure devices, and endobronchial valves) make bronchoscopic management the less invasive, first-choice option, especially those patients who are poor surgical candidates. First described in 2006, BPF occlusion by endobronchial valve is being increasingly reported in the literature, with recent studies demonstrating 48-77% success rate in resolution of BPF (Traveline et al, Chest 2009; Hance et al, Ann Thorac Surg 2015; Cordovilla et al, Arch Broncopneumol 2015).
Although BPF is a complication most commonly associated with lung resection, there are many associated risks that are regularly seen in nonsurgical patients, including malignancy, chronic steroids, and necrotizing lung infections. As critical care physicians, we will definitely care for patients with persistent air leaks and bronchopleural fistulae; it is imperative that we know how to manage them.
[/x_text]
- Shekar K, Foot C, Fraser J, et al. Bronchopleural fistula: an update for intensivists. J Crit Care 2010;25(1):47-55. [PubMed Link]
- Lois M, Noppen M. Bronchopleural fistulas: an overview of the problem with special focus on endoscopic management. Chest 2005; 128:3955-65. [PubMed Link]
- Gaur P, Dunne R, Colson YL, Gill RR. Bronchopleural fistula and the role of contemporary imaging. J Thorac Cardiovasc Surg 2014; 148:341-7. [PubMed Link]
- Baumann MH, Sahn SA. Medical management and therapy of bronchopleural fistulas in the mechanically ventilated patient. Chest 1990;97(3): 721-8. [PubMed Link]
- Giddings O, Kuhn J, Akulian J. Endobronchial valve placement for the treatment of bronchopleural fistula: a review of the current literature. Curr Opin Pulm Med 2014; 20(4):347-51. [PubMed Link]
- Johnson AP, Cavarocchi NC, Hirose H. Ventilator strategies for VV ECMO management with concomitant tracheal injury and H1N1 influenza. Heart Lung Vessel 2015;7(1):74-80. [PubMed Link]
[/x_text]