[x_text]Today we are fortunate to hear from one of our favorite speakers: Dr. Samuel M. Galvagno Jr., Associate Professor of Anesthesiology; Chief, Division of Critical Care Medicine; and Associate Medical Director, SICU at the University of Maryland SOM. Dr. Galvagno has fast become a world renowned expert in the field of shock resuscitation and today will be doing his best to summarize his vast knowledge over some of the most informative 40 minutes you will ever find! Truly this is one of the best talks of the academic year!![/x_text]
[x_text][/x_text][x_text]
Podcast: Play in new window | Download
Subscribe: Apple Podcasts | RSS
[/x_text][x_text class=”left-text “]
Clinical Pearls
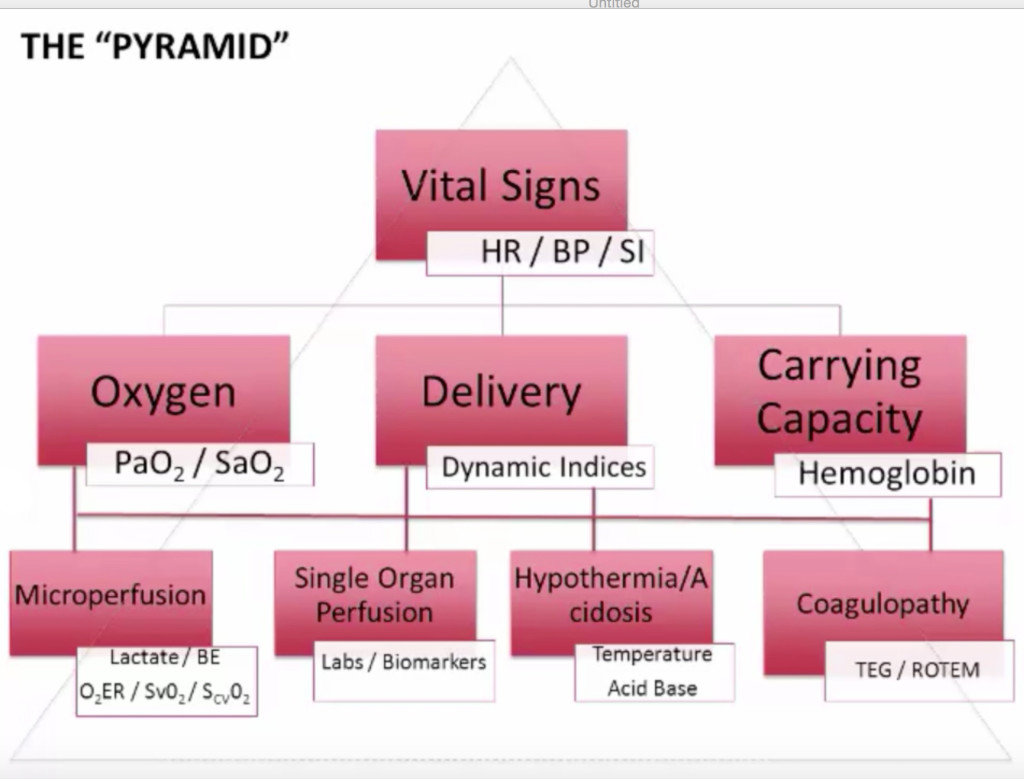
All evaluation starts with the pyramid:
Tips and Tricks
- Prolonged capillary refill is an underused physical exam finding for early shock
- Majority of shock is occult or compensated
- Your HD assessment is one of many end points of resuscitation
Classification of Shock, Four different classes based on:
- Blood loss (Volume and %), HR, BP, Pulse pressure, RR, Urine output (mL/kg), Mental status, and Fluid replacement requirements
- Confounding factors:
- Beta blockers, elderly, young (in compensated shock), anxiety
Oxygen Delivery (DO2)
- DO2 = [(1.34 x Hb x SaO2) + (0.003 x PaO2)] x Cardiac Output x 10
- DO2 = CaO2 x CO
- CO = HR x Stoke Volume
- Stroke Volume affected by 3 factors: Preload, Afterload, Contractility
- CO = HR x Stoke Volume
Upstream Endpoints/Indices
- Hemodynamic Parameters:
- Preload (CVP, PAOP) – Echo is the way to go!
- Afterload (MAP, SVR)
- Pulse pressure variation (PPV)
- Stroke volume variation (SVV)
- Dynamic central arterial elastance (Ea) Ea = PPV/SVV
- Pleth variation index (PVI)
- Dynamic Indices (SV, EF, Ea, PPV, SVV) = Functional hemodynamic monitoring > Static Indices (~CVP)
- Oxygen Delivery Parameters:
- PaO2
- Hemoglobin
- Cardiac Output
- Measures of Vascular Status
- ECHO
- TTE
- TEE
- Minimally invasive monitors (must know the limitations)
- ECHO
Downstream Endpoint/Indices of Perfusion:
- Measuring microcirculation is the goal, but no direct measurement is currently possible!
- SvO2 = SAO2 – [VO2/(1.34 x CO x Hb)] (know for boards)
- Oxygen Extraction Ratio
- Ratio of O2 delivery to uptake
- Normal 20-28%
- >50% = marker of tissue dysoxia
- Approximation: SaO2 – SCVO2
- Lactate
- End product of anerobic glycolysis
- Producted by pyruvate
- Consumed by liver, kidney, other tissues
- If not cleared in 24 hours there is a TERRIBLE outcome expected
- Causes of elevated lactate
- Aerobic Glycolysis
- Beta-2 Stimulation (Epinephrine via Na-K ATPase)
- Enhanced sarcolemmal NaK-ATPase
- Cytokine-stimulated
- Impairment of oxidative phosphorylation
- Inhibition of pyruvate dehydrogenase (sepsis!)
- Liver/kidney disease
- Often it is debated, lactic acid vs SCVO2, but both have their own benefits and should be utilized!
Base Excess:
- Reflects pure metabolic component of acidosis/alkalosis
- Not affected by short-term changes in pCO2
- Amount of base needed to return plasma back to pH 7.4 at standard conditions
- Correlates with mortality, intra-abdominal injury, transfusion requirements
- Failure to normalize in 24hrs: Increased ARDS, MODS, Mortality
- BE ≤ -6 is worrisome
- Pitfalls: Hyperchloremia, Sodium bicarb, Alcohol, ARF, Venous sample (error of close to 2 mmol/L)
Novel Concepts:
- StO2
- NL>65
- Measures Hgb saturation in capillaries, venules, and arterioles
- Focuses on microcirculation with near IR spectroscopy (don’t need a pulse and can be hypothermic)
- Subligual capnography
- Some FDA concerns over tissue damage and infections
- Uses wave lengths to measure microcirculation
- TEG/ROTEM
- Eval for end points of resuscitation for coagulopathy
- Need to follow serial measurements to eval for minute to minute changes
[/x_text]
[x_text]Suggested Reading
- Tseng GS, Wall MH. Endpoints of resuscitation: what are they anyway? Semin Cardiothorac Vasc Anesth. 2014 Dec;18(4):352-62.[PubMed Link]
- Joshi R, de Witt B, Mosier JM. Optimizing oxygen delivery in the critically ill: the utility of lactate and central venous oxygen saturation (ScvO2) as a roadmap of resuscitation in shock. J Emerg Med. 2014 Oct;47(4):493-500.[PubMed Link]
- Kraut JA, Madias NE. Lactic acidosis. N Engl J Med. 2014 Dec 11;371(24):2309-19.[PubMed Link]
[/x_text]