Today we welcome a close friend and colleague from Washington DC: Christian Woods, MD. Dr. Woods has many jobs including: associate medical intensive-care unit director, director of the Pulmonary Fellows’ Ambulatory Clinic; AND attending physician in both Pulmonary/Critical Care and Infectious Diseases for the Washington Hospital Center. In addition to his all these clinical responsibilities, he is also an assistant professor of Infectious Diseases, at Georgetown University Medical Center. With this immense background we begged him to speak to us on the very difficult topic of managing a critically ill HIV patient. He has spent years cultivating this expertise and in just 50 minutes he manages to pass along so much knowledge you might just have to watch several times to catch them all!!
Podcast: Play in new window | Download
Subscribe: Apple Podcasts | RSS
Clinical Pearls
#1 thing to keep in ming: most admissions for HIV pts are for non-HIV affected long standing medical issues (COPD, HTN)
Powell K, et al. Chest. 2009 Jan;135(1):11-7.
HIV Specific Issues:
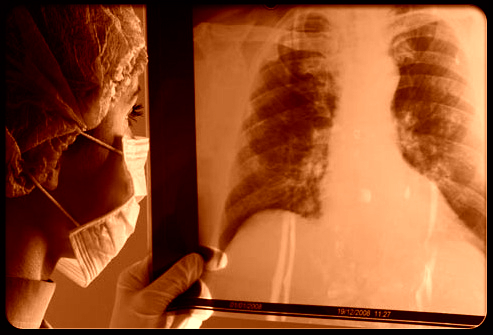
- PCP
- Mod-Severe: IV Bactrim
- Mild: PO Bactrim
- Steriods for PaO2<70 mmHg or A-a gradient >35 mmHg
- 40mg BID x 5, 40mg Qday x 5, 20mg Qday x 11
- why? can ½ the amount of resp failure, and ½ the risk of mortality
- Sulfa allergy?
- Mod-Severe: IV Pentamidine, watch QT prolongation and hypoglycemia OR PO Primaquine and Clinda
- Mild: PO TMP + Dapsone, PO Primaquine + Clina, or PO Atovaquone
- Watch for PTX, very common with PCP and has a mortality of 50% (vs 25% in HIV w/o PCP).
- ECMO + PCP? Better if cannulated early, but limited data!
- Crypto
- Liposomal amphotericin + Flucytosine (adjusted by renal failure) for at least 2 weeks
- Delay the start of HAART – do better waiting 5 weeks (especially with WBC<20 cells/uL which is a prognosticator for poor outcome)
- Watch for high CSF pressures + neurological deficits (ex: blindness)
- If pressure >25 cm H2O with symptoms, goal is to decrease to 50% of initial pressure with serial LPs until below 20 cm H2O
- Liposomal amphotericin + Flucytosine (adjusted by renal failure) for at least 2 weeks
- HAART Drug reactions:
- Ritonavir and Fluticasone + any cessation of treatment = adrenal insufficiency
- Beclamethasone is safer
- Why? Fluticasone has a longer half life (10.5 hours), has a larger VOD, & most suppressive on HPA axis
- Abacavir reaction- Hypotension in 5-8% of population
- Initial symptoms are non-specific, but 25% of re-challenges will be hypotensive
- Need to test prior to starting (HLA B5701)
- SJS
- Think Bactrim, Efavirenz, Nevirapine
- Ritonavir and Fluticasone + any cessation of treatment = adrenal insufficiency
- Immune reconstitution syndrome (IRIS)
- Worsening of preexisting infections following HAART initiation
- Present with severe exacerbation of underlying infection
- Criteria:
- CD4 <100 (unless Tb)
- + Virologic and immune response
- Competing diagnoses are excluded
- Manifestations consistent with inflammatory condition
- Temporal association to HAART (2 months)
- Risks
- Low CD4, high viral load
- New HAART
- Short interval btw opportunistic infection treatment and HAART
- Treatment
- Tx underlying infection + continue HAART + anti-inflammatory tx
- Worsening of preexisting infections following HAART initiation
Suggested Reading
- Powell K, Davis JL, Morris AM, Chi A, Bensley MR, Huang L. Survival for patients With HIV admitted to the ICU continues to improve in the current era of combination antiretroviral therapy. Chest. 2009 Jan;135(1):11-7.[PubMed Link]