Today we have Dr. Samuel Tisherman, the current Director of the Center for Critical Care and Trauma Education here at the UMMC. Dr. Tisherman is a recent transplant from the University of Pittsburgh where he was the Director of the Multidisciplinary Critical Care Training Program and program director for the Surgical Critical Care Fellowship. If all that wasn’t enough, in addition to his numerous teaching awards, he was also elected to the prestigious University of Pittsburgh School of Medicine Academy of Master Educators. So obviously with this phenomenal educational pedigree, Dr. Tisherman is the perfect individual to lead a discussion on the one topic we only get one shot to master: Emergency and Surgical Airways! Trust me, this talk WILL save someone’s life in the next week!!
Podcast: Play in new window | Download
Subscribe: Apple Podcasts | RSS
Clinical Pearls (Special thanks to Raffy Trinidad, MD)
When to attempt a surgical airway?
- Emergency Situations
- Elective Situations
- Special Situations
- Complications
Always remember: the inability to intubate the trachea is the only indication for creating a surgical airway!
Requirements:
- Best intubator – Anesthesia attending
- Surgical airway – Trauma attending
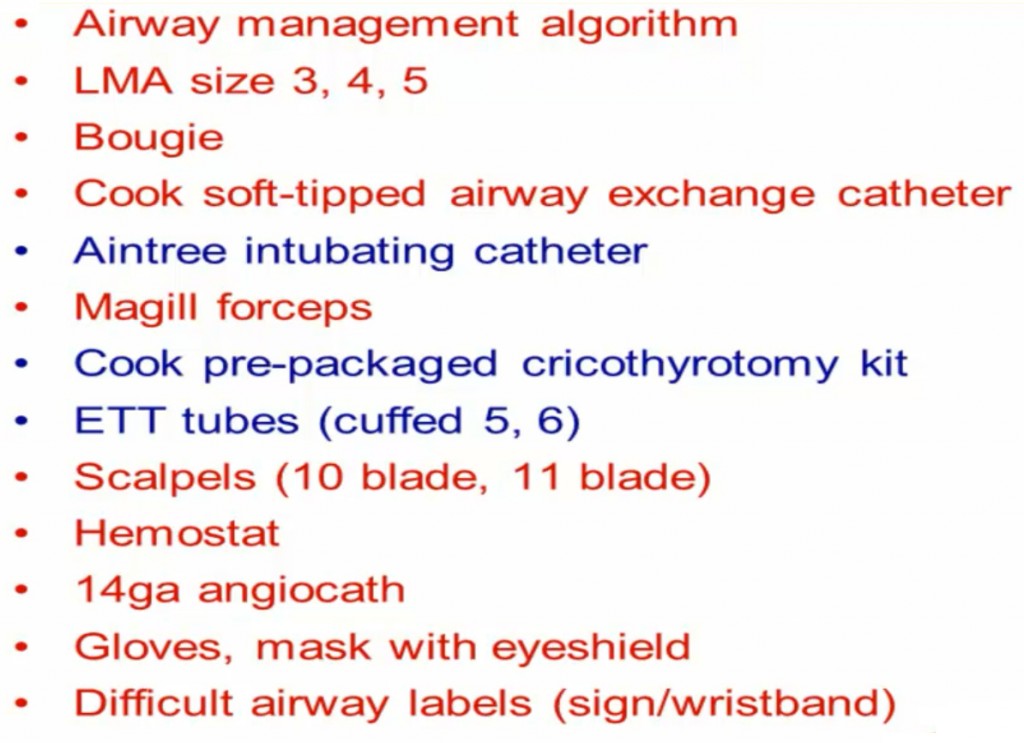
- Difficult Airway Equipment
Options:
- Needle cricothyroidotomy
- Have to have direct wall oxygen
- Pitfalls:
- Pt selection: need a special kit, need a compliant pt
- Procedurally difficult: easy to pierce the back wall of trachea, can cause SQ emphysema
- Catheter is kinked easily
- Difficult to use with increased secretions or with complete airway obstruction
- Difficult to remove CO2
- Surgical cricothyroidotomy
- Requires: hands, knife, tube!
- landmarks: thyroid cartilage, cricothyroid membrane
- Stand to right of pt (if right handed)–> grab thyroid and don’t let go–>vertical incision (avoid blood vessels)–> dilate with finger–> bougie–> ETT
- Pitfalls:
- CI in pediatrics (narrowest part of airway, can cause stenosis)
- Pt selection: most pts are already apniec and stress level is high
- Anatomy: destructive maxillofacial/neck injuries, poor landmarks
- Requires: hands, knife, tube!
- Awake tracheostomy
- Must be: compliant and breathing spontaneously
Tracheostomy vs Cricothyroidotomy
- Cricothyoroidotomy is easier because:
- Cricothyroid membrane is more superficial, thus easier to target
- Has less bleeding
- Causes less recurrent laryngeal injury, pneumothorax, etc.
- Requires less instruments, assistance, and lighting
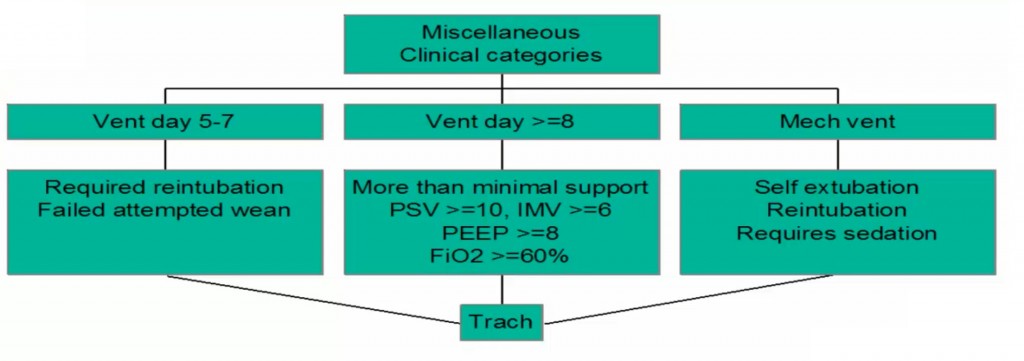
When to trach?
Percutaneous or Open?
- Open is more advantageous because
- Faster with less bleeding and smaller scars
- Far easier to learn and requires less assistance
- Requires fewer instruments and less lighting
- Less infection and/or tracheal erosion (theoretical)
- Would not use open on an obese patient
Pitfalls of any tracheostomy:
- Trachea-Innominate artery fistula
- Peak incidence 1st to 2nd week post-op (0.3% incidence)
- Juxtaposition of trachea and innominate artery –> pressure necrosis from tube
- Prevention
- Avoid neck hyperextension and accurately place the trach 2nd or 3rd ring
- Monitor cuff pressure<20mm Hg
- Avoid tight closure of skin incision
- Promptly treat all peristomal infections
- Use long flexible connecting tubing and avoid a stiff trach tube
- Emergency treatment:
- Overinflation of cuff OR remove trach–> intubate from above–> stick your finger in and hold pressure at the bleeding site (Utley maneuver)
Suggested Reading
- Berkow LC, Greenberg RS, Kan KH, Colantuoni E, Mark LJ, Flint PW, Corridore M, Bhatti N, Heitmiller ES. Need for emergency surgical airway reduced by a comprehensive difficult airway program. Anesth Analg. 2009 Dec;109(6):1860-9.[PubMed Link]
- Young D, Harrison DA, Cuthbertson BH, Rowan K; TracMan Collaborators. Effect of early vs late tracheostomy placement on survival in patients receiving mechanical ventilation: the TracMan randomized trial. JAMA. 2013 May 22;309(20):2121-9.[Pubmed Link]