We are fortunate to lure Dr. Michael Winters to the auditorium for another brilliant talk. Dr. Winters finished as one of the first EM/IM/CCM at the University of Maryland and he was wise enough to stay and serve as the Medical Director of the ED and has fast become one of the most well known and widely published experts in the field of practicing critical care medicine in the emergency room. You cannot find a more knowledgable and dedicated educator, so I hope you take advantage of this fantastic lecture! Your patients will thank you for it!!
Clinical Pearls (Assisted by Dr. Raffy Trinidad)
Most Important Factors
- Team Leadership
- Hemodynamic Directed Resuscitation
- High Quality CPR
- Early Defibrillation
- Medications
- Novel Therapies
- Post Arrest Care
1) Team leadership
- Deficits in leadership can cost lives
- ex: poor performance of CPR, decreased ROSC, decreased survival
- Benefits:
- Good leadership –> establish ROSC faster
- Proper planning (ex: role assignment) –> reduced hands-off time, less interruption, faster treatment completion
- Improved communication –> accuracy of team leader communications linked to errors
- Roles of the team leader:
- ensures delivery of adequate compressions
- minimize interruptions
- avoid excessive ventilation
- What can you do? Take charge!
- direct all components of resuscitation
- assign tasks
- communicate clearly
- be decisive
2) Hemodynamic directed resuscitation
- Survival dependent upon restoring myocardial blood flow
- Keep coronary blood flow (CPP) >20mmHg, three ways to check
- DBP – RAP (or CVP), caveat: need A-line and central line
- DBP>25mmHg, just need A-line
- ETCO2>20
- May use these parameters to optimize CPR, guide vasopressor use, and detect ROSC
- Keep coronary blood flow (CPP) >20mmHg, three ways to check
3) High quality CPR
- Rate: 100-120/min
- Depth: 5-6 cm (2-2.4 inches)
- Allow full chest recoil
- Avoid leaning
- Chest compression fraction > 60% (minimize interruptions)
- Eliminate pulse checks
4) Early defibrillation
- Hands off for shock, charge while compressions are occurring
- Limit perishock pause to <10s
5) Medication
- Vasopressors
- Increase aortic pressure
- Improve CPP
- Improve cerebral perfusion pressure
- No definitive evidence that any vasopressor agent improves long-term survival
- Epinephrine
- Decreases microcirculatory cerebral flow
- Increased myocardial O2 consumption
- Increased post-defib ventricular arrhythmias
- Increased post-ROSC myocardial dysfunction
- Standard dose (1mg q3-5mins) MAY be reasonable
- Vasopressin – not recommended
6) Novel therapies
- ECPR not universally accepted
- best outcomes: witnessed arrest, bystander CPR w/in mins, shockable rhythm, short EMS transport time, short time to ECMO, emergent hypothermia, and PCI
7) Post arrest goals
- Optimize oxygenation and ventilation
- Decrease FiO2 for O2sat>94%
- Goal: PCO2 35-45; ETCO2 30-40
- Optimize hemodynamics
- Targeted temp management
- Comatose adult patients with ROSC after cardiac arrest (32-36C for 24 hours)
- No benefit of endovascular over surface cooling
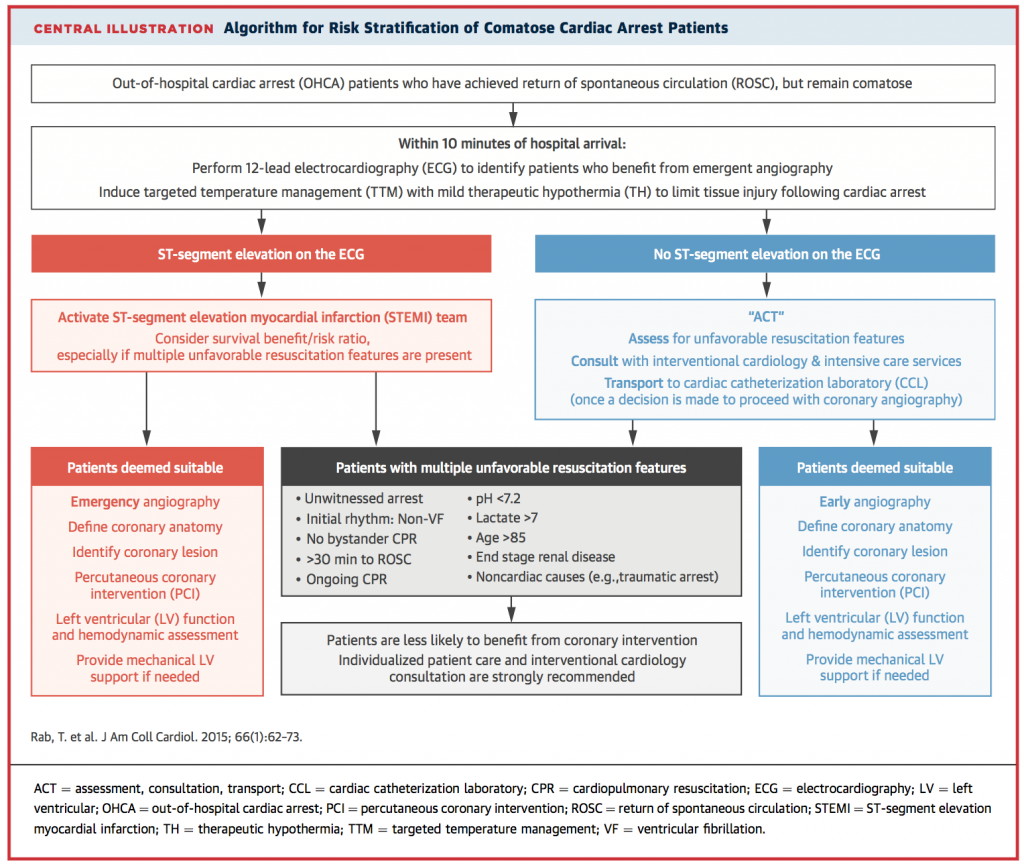
- Emergent PCI
- STEMI, NSTEMI with hemodynamic instability or refractory VF/Vfib or ongoing ischemia
Suggested Reading
- Rab T, Kern KB, Tamis-Holland JE, Henry TD, McDaniel M, Dickert NW, Cigarroa JE, Keadey M, Ramee S; Interventional Council, American College of Cardiology. Cardiac Arrest: A Treatment Algorithm for Emergent Invasive Cardiac Procedures in the Resuscitated Comatose Patient. J Am Coll Cardiol. 2015 Jul 7;66(1):62-73.[PubMed Link]
- Meaney PA, Bobrow BJ, Mancini ME, et al. Cardiopulmonary resuscitation qual- ity: improving cardiac resuscitation outcomes both inside and outside the hospital: a consensus statement from the American Heart Association. Circu- lation 2013;128:417–23.[Circulation Link]
- Link MS, Berkow LC, Kudenchuk PJ, Halperin HR, Hess EP, Moitra VK, Neumar RW, O’Neil BJ, Paxton JH, Silvers SM, White RD, Yannopoulos D, Donnino MW. Part 7: Adult Advanced Cardiovascular Life Support: 2015 American Heart Association Guidelines Update for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2015 Nov 3;132(18 Suppl 2):S444-64.[PubMed Link]