Today we welcome back Dr. Nirav Shah, program director for the Pulmonary and Critical Care Fellowship program at the University of Maryland Medical Center. Today Dr. Shah takes us back to the basics of ventilator use. Even the experts in the audience will find tips and tricks to take back to the ICU in order to improve patient care. And for all the budding intensivists out there, this is a talk you cannot miss!!
Podcast: Play in new window | Download
Subscribe: Apple Podcasts | RSS
Clinical Pearls (Assisted by Dr. Helen Prevas)
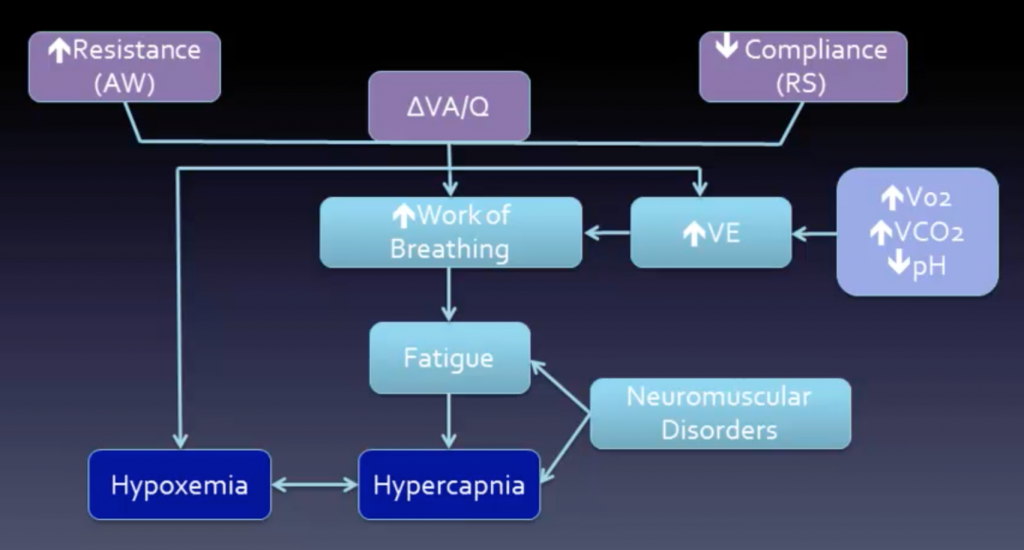
Respiratory failure:
- Type 1: hypoxic
- #1 cause V/Q mismatch
- Decreased ventilation (airway, ILD)
- Increased perfusion to normally ventilated lung (PE)
- Shunt
- ARDS, PNA, edema
- #1 cause V/Q mismatch
- Type 2: hypercarbic
- Need to correct decreased alveolar hypoventilation
- Increase minute ventilation +/- decrease dead space (if hypoxic, will correct with oxygenation)
- Need to correct decreased alveolar hypoventilation
- Treatment:
- Reverse cause + positive pressure
- Decrease work of breathing
- Restore adequate gas exchange
- Noninvasive (NIV)
- CPAP, BiPAP, cuirass
- Invasive (ETT or tracheostomy)
- volume, pressure, hybrid, or “novel” modes (i.e., APRV, NAVA)
- Reverse cause + positive pressure
Goals:
- Ventilation
- Acceptable pCO2 + pH
- Goal Pplat <30
- Decrease auto-PEEP (breath stacking)
- Oxygenation
- Goal SpO2 >88% on FiO2 <60%
- Optimal delivery of O2: (DO2) = CO x (1.34 × Hb × SaO2) + (0.003 × PaO2)
- ARDS
- tidal volume ≤ 6 cc/kg IBW (based on height)
- Conservative fluids
- Avoid VILI
Ventilator Definitions:
- Control
- How a breath is delivered (V vs. P vs. dual)
- Triggering
- When inspiration starts (flow or pressure)
- Cycling
- What determines switch from insp to exp
- Time or flow sensed
- Breaths
- Mandatory, assisted, spontaneous
- Flow pattern
- Often set by the method of control
- Sinusoidal, accelerating, constant (square), decelerating
- Mode or breath pattern:
- Spontaneous, assist control (AC), intermittent mandatory ventilation (IMV)
- Pressure supported (PS) or volume supported (VS)
- Scalar
- Waveforms that plot pressure, flow, or volume vs time on the ventilator screen
- Loops
- Pressure or flow vs. volume (look like PFTs upside down)
Waveforms:
- Allow provider to:
- Assess real time changes in patient condition
- Optimize vent settings and treatment
- Determine effectiveness of vent
- Detect adverse events
- Decrease risk of mechanical complications
- Pressure waveforms
- Diagnose: air trapping, obstruction, dyssynchrony, pressures (i.e., plateau or end inspiratory hold), triggering, bronchodilator response
- Area under the pressure curve = Alveolar distending pressure
- Flow waveforms
- Detect air trapping, obstruction, bronchodilator response, triggering, dyssynchrony
- Square
- Pressure rises (higher peak inspiratory pressure)
- Decelerating
- Pressure constant
- Plateau pressure is greater for Square vs. Decelerating with same volume
- Volume waveform
- Can detect air trapping, leak, tidal volume, dyssynchrony
Ventilator adjustments:
- I (inspiratory) time
- Set for PRVC and PC, VC on some vents (otherwise set flow)
- PS: cycles once falls below set % of peak flow (decelerating flow)
- Decrease Ti: less autoPEEP, decrease CV effects
- Increase Ti: improves oxygenation
- Set for PRVC and PC, VC on some vents (otherwise set flow)
- Trigger sensitivity
- Increased sensitivity can lead to autotrigger/false triggering (water in circuit, heartbeat)
- Rise time
- Rate of rise of pressure (PC) or flow (VC)
- Short: may be uncomfortable, but can lead to decreased inspiratory workload
- Reduced VILI (biotrauma)
- Long: decreased Tv in pressure mode (less time at set pressure) or increased pressure in volume mode (to reach target volume)
- Short: may be uncomfortable, but can lead to decreased inspiratory workload
- Rate of rise of pressure (PC) or flow (VC)
Troubleshooting:
- Dx increased peak without change in Pplat
- Increased resistance → obstruction, bronchospasm, biting, foreign body
- Dx increase peak and Pplat
- Decreased lung compliance (or increased Vt)
- PTX, abdominal HTN, ARDS, edema
- Decreased lung compliance (or increased Vt)
- How to detect AutoPEEP
- Flow not returning to 0 before next breath
- Area under inspiratory curve not equal to area under expiratory curve
- Dyssynchrony (double triggering)
- Treating airway obstruction:
- Bronchodilators
- Suction
- Prolong expiration
- Decrease I time
- Increase flow
- Sedate if necessary
- Increase extrinsic PEEP (2/3 intrinsic)
Suggested Reading
- Bone RC, Eubanks DH, Gluck E. Beyond the basics: operating the new generation of ventilator. A look at the features and functions of these units. J Crit Illn. 1992 May;7(5):770-82; 787-8.[PubMedLink]
- Bone RC, Eubanks DH. The basis and basics of mechanical ventilation. Dis Mon. 1991 Jun;37(6):321-406.[PubMed Link]
- Carbery C. Basic concepts in mechanical ventilation. J Perioper Pract. 2008 Mar;18(3):106-14.[Pubmed Link]