Today we welcome one of the gurus in anti-coagulant reversal, John J. Lewin, PharmD, MBA, FASHP, FCCM, FNCS, BCCCP. Dr. Lewin is a pharmacy specialist out of Johns Hopkins where he acts as the Division Director for Critical Care & Surgery Pharmacy Services; an Associate Professor of Anesthesiology & Critical Care Medicine; AND he continues to teach as a Clinical Professor at the University of Maryland School of Pharmacy. Dr. Lewin recently published one of the recent landmark articles in the field of Neurocritical care: “Guideline for Reversal of Antithrombotics in Intracranial Hemorrhage”. Today he is gracious enough to spend 60 minutes with us, and not a second can be missed if you EVER expect to take care of a patient with a head bleed on AC!!
Podcast: Play in new window | Download
Subscribe: Apple Podcasts | RSS
Clinical Pearls (Summary assisted by by Dr. Faith Armstrong)
Quick pearls:
- Antithrombotic ICH is expected to become more common and antithrombotic-associate ICH has a higher risk of hematoma expansion, higher mortality, and worse outcome
- Most of our epidemiologic data is specific to warfarin
- Rates of ICH with novel AC are lower, but we don’t have very effective methods of reversal
Specific agents:
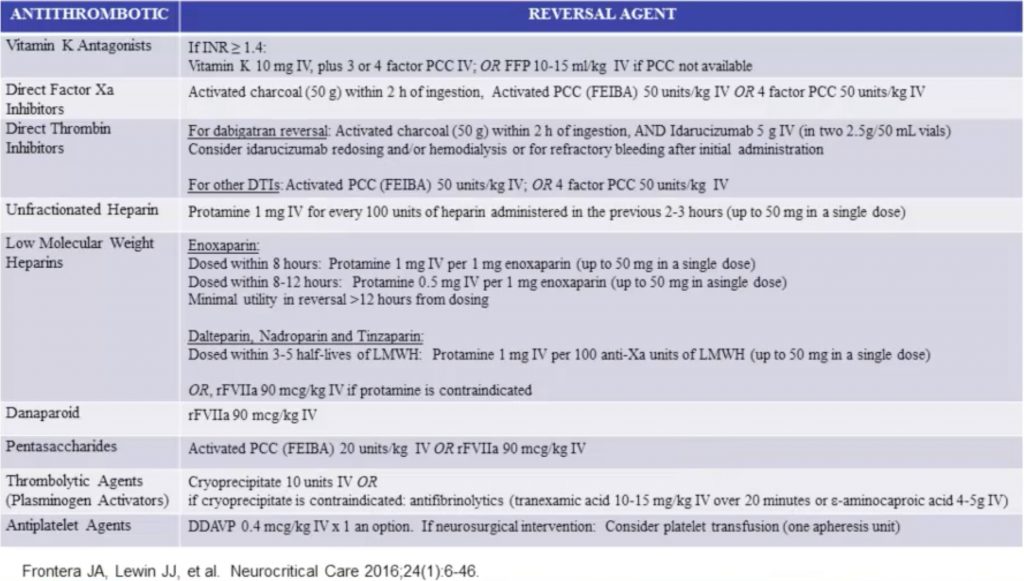
- Vitamin K Antagonists (i.e. Warfarin): inhibits vitamin K oxide reductase, therefore inhibition of Facts II, VII, IX, and X
- Doubles risk of IPH, causing 12-14% of all IPH (with risk increasing with INR lvl!)
- Antidotes:
- Vitamin K
- It can take up to 24 hours to decrease INR with Vit K alone
- Vit K in addition to PCC or FFP is needed to provide long-lasting INR correction
- Low risk of anaphylaxis which can be mitigated by diluting it and infusing over 10-15 minutes
- Recommended dose is 10mg (unless re-anticoagulation is needed rapidly for whatever reason, in which a lower dose would be beneficial); IV route is preferred
- It can take up to 24 hours to decrease INR with Vit K alone
- Factor replacement
- Vitamin K
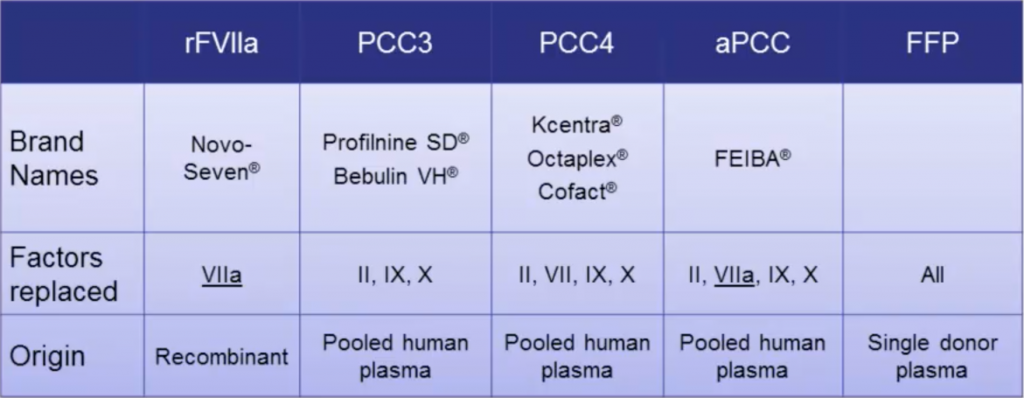
- PCC
- Pros: lower volume, fast reconstitution, more rapid INR correction, lower infection risk
- Cons: expensive, not widely available, some must be re-dosed
- FFP
- Pros: widely available, less expensive
- Cons: needs to be thawed/matched, slower correction, risk of TRALI/TACO
- Two RCTs: no difference in thrombosis rates (3-8%)
- INCH trial: new 2016 study showing PCC is much more rapid and effective
- Less hematoma expansion with PCC which stopped the study!
- Ideal Strategy
- Give PCC (rather than FFP) for INR correction WITH vit K 10mg IV
- Suggest PCC4, but low quality evidence
- PCC dosing should be weight-based & vary according to admission INR and type of PCC used
- Repeat INR testing 15-60 min post-PCC and every 6-8h for 24h
- Subsequent tx should be guided by INR (high risk for DIC with re-dosing)
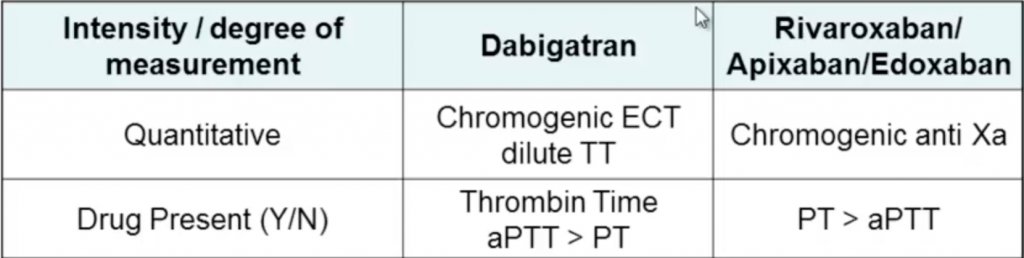
- Direct Inhibitors: Bind to and directly inhibit Factors (Factor Xa inhibitor- Rivaroxiban/Apixaban/Edoxaban) and Thrombin (Factor IIa inhibitor- Dabigatran)
- Dabigatran (thrombin inhibitor)
- New FDA approved agent: Idarucizumab (monoclonal antibody)
- RRT will remove the drug as well, but drug levels will rebound
- Ideal Strategy
- Assess time of last ingestion (T1/2 ~12 hrs), renal function, medication interactions
- Reversal should be guided by bleeding and not lab testing
- Activated charcoal (50g) to intubated patients with ICH and/or those at low risk for aspiration who present <2h post-ingestion
- CRRT is usefel due to low MW and low protein bound status
- Administer Idarucizumab (5g IV two divided doses) if dabigatran was administered within a period of 3-5 half lives and no renal failure OR if there is renal insufficiency leading to continued drug exposure
- Assess time of last ingestion (T1/2 ~12 hrs), renal function, medication interactions
- New FDA approved agent: Idarucizumab (monoclonal antibody)
- Rivaroxiban/Apixaban/Edoxaban (Factor Xa inhibitors)
- Potential reversal options:
- Activated charcoal within 2h of intake
- Animal studies showing partial correction of lab abnormalities with PCC, aPCC, rFVIIa
- Upcoming reversal agents in clinical trials (Andexanet-recombinant Xa, Aripazine)
- Ideal Strategy
- Discontinue agent
- Activated charcoal as above
- PCC4 (50 U/kg) or aPCC (50 U/kg) if ICH occurred within 3-5 half lives OR in context of liver failure (based on very limited data)
- Await trial results for novel reversal agents
- Potential reversal options:
- UFH:
- Protamine for UFH reversal (1mg neutralizes 80-120 units of heparin)
- Dose according to amount of heparin received in the past 2-3 hours with 1mg/100 U heparin received (max single dose of 50mg)
- Protamine for UFH reversal (1mg neutralizes 80-120 units of heparin)
- LMWH:
- Protamine with dose based on timing of last LMWH dose
- If LMWH w/in 8h: 1mg protamine/1mg LMWH received
- If LMWH w/in 8-12h: 0.5mg Protamine/1mg LMWH received
- If Protamine contraindicated, can use rFVIIa (90mcg/kg IV)
- Andexanet? Stay tuned…..
- Protamine with dose based on timing of last LMWH dose
- Pentasaccharides (Fondaparinux, Idraparinux)
- Protamine ineffective
- aPCC (20 IU/kg) for reversal
- If not available then rFVIIa (90mcg/kg)
- Thrombolytics
- Alteplase, Reteplase, and Tenecteplase bind preferentially to fibrin-bound plasminogen
- Urokinase and Streptokinase bind equally to free and fibrin-bound plasminogen
- Will cause a reduction in Fibrinogen (may be a marker of bleeding risk) and anti-platelet effects for ~ 12 hours
- Antidotes:
- Cryoprecipitate
- Fibrinogen, FVIII, FXIII, fibronectin, vWF
- Target fibrinogen >100 mg/dL
- Antifibrinolytics
- Bind to and inactivate plasmin and plasminogen preventing fibrinolysis
- Amiocaproic acid & Tranexamic acid (TXA)
- Cryoprecipitate
- Ideal Strategy
- Cryoprecipitate (10 units) who have received a thrombolytic agent in past 24h
- Check fibrinogen levels after administration for goal >100
- If cryo contraindicated or not available, TXA (10-15mg/kg over 20 min) or amiocaproic acid (4-5g IV) may be used
- Cryoprecipitate (10 units) who have received a thrombolytic agent in past 24h
- Alteplase, Reteplase, and Tenecteplase bind preferentially to fibrin-bound plasminogen
- Antiplatelets
- Ideal Strategy
- No routine platelet transfusions unless undergoing a neurosurgical procedure
- PATCH trial:
- Pts on anti-platelet therapy with an acute CVA
- Odds of death was higher in patients who received platelets!
- Desmopressin
- No benefit found in case series, however very little harm
- Ideal Strategy
Suggested Reading
- Frontera JA, Lewin JJ 3rd, Rabinstein AA, Aisiku IP, Alexandrov AW, Cook AM, del Zoppo GJ, Kumar MA, Peerschke EI, Stiefel MF, Teitelbaum JS, Wartenberg KE, Zerfoss CL. Guideline for Reversal of Antithrombotics in Intracranial Hemorrhage: A Statement for Healthcare Professionals from the Neurocritical Care Society and Society of Critical Care Medicine. Neurocrit Care. 2016 Feb;24(1):6-46. [PubMed Link]
- Baharoglu MI, Cordonnier C, Al-Shahi Salman R, de Gans K, Koopman MM, Brand A, Majoie CB, Beenen LF, Marquering HA, Vermeulen M, Nederkoorn PJ, de Haan RJ, Roos YB; PATCH Investigators. Platelet transfusion versus standard care after acute stroke due to spontaneous cerebral haemorrhage associated with antiplatelet therapy (PATCH): a randomised, open-label, phase 3 trial. Lancet. 2016 Jun 25;387(10038):2605-13. [PubMed Link]
- Pollack CV Jr, Reilly PA, Eikelboom J, Glund S, Verhamme P, Bernstein RA, Dubiel R, Huisman MV, Hylek EM, Kamphuisen PW, Kreuzer J, Levy JH, Sellke FW, Stangier J, Steiner T, Wang B, Kam CW, Weitz JI. Idarucizumab for Dabigatran Reversal. N Engl J Med. 2015 Aug 6;373(6):511-20. [PubMed Link]
- Steiner T, Freiberger A, Griebe M, Hüsing J, Ivandic B, Kollmar R, Pfefferkorn T, Wartenberg KE, Weimar C, Hennerici M, Poli S. International normalised ratio normalisation in patients with coumarin-related intracranial haemorrhages–the INCH trial: a randomised controlled multicentre trial to compare safety and preliminary efficacy of fresh frozen plasma and prothrombin complex–study design and protocol. Int J Stroke. 2011 Jun;6(3):271-7. [PubMed Link]