Today we welcome Giora Netzer M.D., M.S.C.E., Associate Professor of Medicine here at the University of Maryland Medical Center. Dr. Netzer was trained at the great bastion of intensive care medicine, the University of Pennsylvania, where he also earned a master’s degree in clinical epidemiology. Since joining the University of Maryland Pulmonary and Critical Care Medicine department he has proven to be one the greatest minds the ICU has to offer, earning him the title: Wiki-Netzer. His passion for knowledge led to his appointment as the Director of Clinical Research and has yielded a tremendous breadth of publications. Today he focuses on his true passion: how to assist family members care for their loved ones both in the ICU and in the post-ICU setting. Trust me, this is a topic that is often overlooked and one that can truly mean life or death for your patients! You cannot miss it!!
Clinical Pearls (Assisted by Jessica Buchner, MD)
- Family
- A group of individuals who share each other’s lives
- SCCM does not require this to be a “blood relative”
- Majority of decision-making in ICU is made by surrogates
- Need to collaborate and share decision making btw multiple members of families
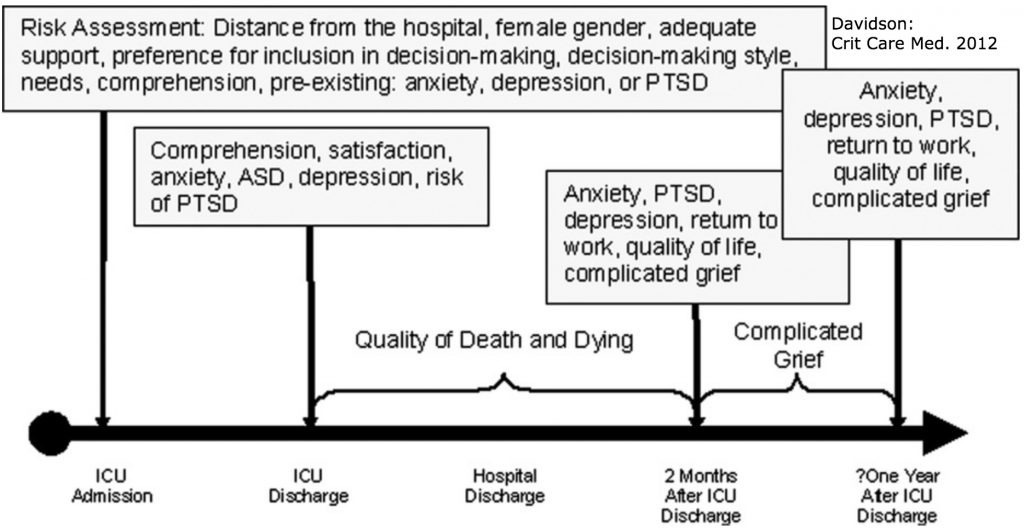
- Leads to stress, depression, even PTSD among family members
- 44% of caregivers are depressed and possess low problem solving (correlates with depression)
- Good communication matters
- Miscommunication increases length of stay, financial burden, family conflict, increased risk of PTSD
- Treatment team must be aware of the cultural ideals held by the family (leads to effective communication)
- Communicators must anticipate the grief of the receivers (serves as a cognitive barrier)
- Families often experience learned helplessness, maladaptive reasoning- “learned helplessness”
- Stress that cannot be controlled → disengage → withdrawal
- Level of stress correlates to “learned helplessness”
- Families often experience learned helplessness, maladaptive reasoning- “learned helplessness”
- High levels of stress cause family members to have excessive daytime sleepiness, and decreased quality of life (Int Care Med, 2014)
- “Sleepiness” leads to cognitive blunting and decreased executive functioning
- Family members are often internally conflicted about feeling blame for the patient’s death
- Worried about the reaction of other family members in regards to their decisions
- Families often misinterpret prognostic information:
- Optimism bias (“he’s a fighter”, faith-based hope, etc.)
- Framing bias (how data are presented changes interpretation)
- Emotional vs logical reasoning (in a highly emiotionally charged state you are not in a place to make adequate decisions)
- Conflict between providers and family members increases burnout rates
- >40% of ICU physicians and nurses report conflict btw staff and families as a source of conflict
- Futile care is often perceived as hurtful to patient and a waste of resources
- Family-centered care improves overall outcomes
- Increased early mobilization and lessens ICU burden
- Family members must be thought of as a part of the treatment team
- Majority of ICUs have visitor restrictions and instead should build more family presence into policy
- How to remedy the problems:
- Open visitation (unlimited hours)
- Dedicated family meeting room
- “Family support zones”
- Provision of basic needs for families
- Dedicated areas near the ICU for vending machines, shower facilities, group kitchen
- Hospital laundry access
- Sleeping space in the room
- Bedside rounds
- Including bed side engagement
- Decreases family stress
- Increases satisfaction scores
- More frequent family discussions
- Utilize families to help with bedside treatments such as mouth care, talk therapy, passive range of motion
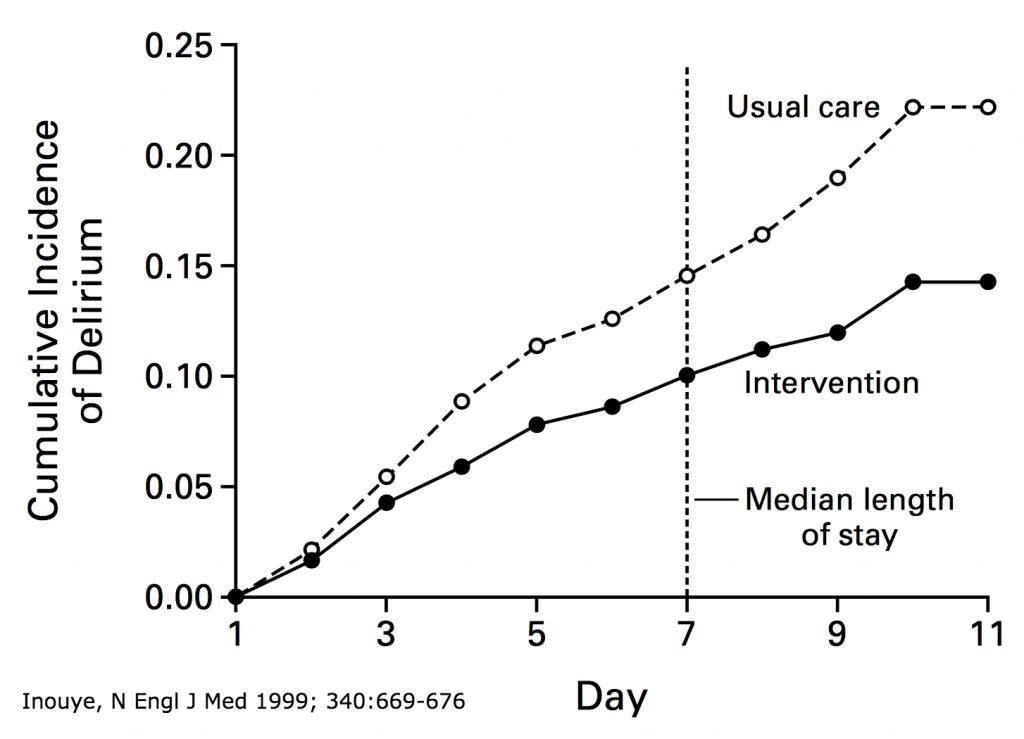
- With similar interventions there is decreased delirium and thus improved outcomes:
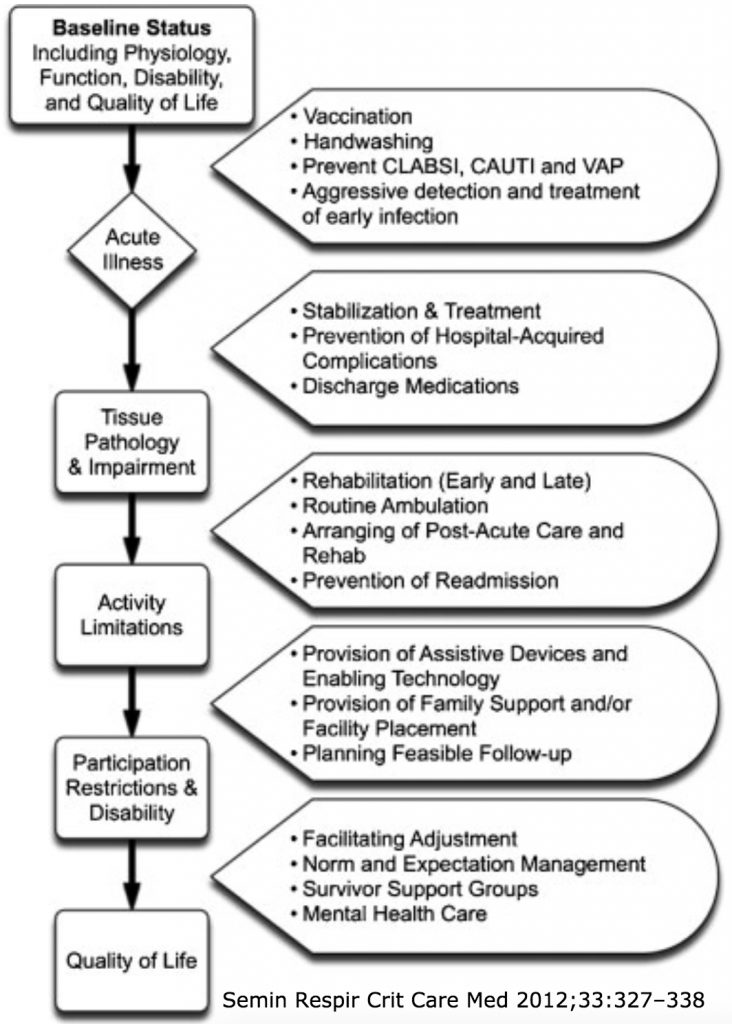
- Over the next several years we will see more ICU survivors (based on modern treatment techniques)
- We need more resources dedicated to helping survivors and their families cope:
- Post-intensive care syndrome
- Cognitive and physical dysfunction, seen both in patients and their families
- Critical illness neuropathy/myopathy
- Post-intensive care syndrome
- We need more resources dedicated to helping survivors and their families cope:
- SCCM THRIVE initiative: optimize care for ICU survivors while in the hospital and after discharge
Suggested Reading
- Davidson JE, Jones C, Bienvenu OJ. Family response to critical illness: postintensive care syndrome-family. Crit Care Med. 2012 Feb;40(2):618-24. [PubMed Link]
- Verceles AC, Corwin DS, Afshar M, Friedman EB, McCurdy MT, Shanholtz C, Oakjones K, Zubrow MT, Titus J, Netzer G. Half of the family members of critically ill patients experience excessive daytime sleepiness. Intensive Care Med. 2014 Aug;40(8):1124-31. [PubMed Link]
- Netzer G, Sullivan DR. Recognizing, naming, and measuring a family intensive care unit syndrome. Ann Am Thorac Soc. 2014 Mar;11(3):435-41. [PubMed Link]