Today we are pleased to feature a groundbreaking talk by a recent addition to the Shock Trauma faculty, Samuel Tisherman, MD, FACS, FCCM. Dr. Tisherman is a Professor of Surgery and Director of the Division of Critical Care and Trauma Education here at the University of Maryland. He is also one of the worlds foremost experts on using hypothermia in the resuscitation of trauma patients. Today he gives a preface for his revolutionary EPR-CAT trail. You will want to be on the cutting edge of this revolutionary concept!
Clinical Pearls
Accidental Hypothermia
- Exposure hypothermia
- Heat loss by conduction, convection, evaporation, or radiation to the environment
- Risks: #1 Alcohol
- Decreased shivering
- Increased vasodilation
- Poor nutrition → less heat generation
- Poor judgement
- Contributing factors:
- Exposure, age (decreased thermoregulation), nutrition, health (neuro disease, endocrinopathies, sepsis), skin conditions (burns), medications (Benzos, TCA, barbs)
- Risks: #1 Alcohol
- Need a core temperature!
- Then you need to stage the patient for management:
- Heat loss by conduction, convection, evaporation, or radiation to the environment
- Organ systems affected by Hypothermia:
- “Umbles”
- Stumbles
- Mumbles
- Fumbles
- Grumbles
- CNS changes
- Agitation → lethargy → coma
- Decreased metabolism, 6-7% per ºC (used in TTM)
- EEG silence at 19-20°C
- Need to rule out other neuro pathologies (bleeds, ischemia)
- Respiratory
- Tachypnea → bradypnea → apnea
- Bronchorrhea, pulmonary edema
- Intubate! – airway protection and apnea
- Cardiac
- Osborne (“J”) waves
- Arrythmia progression: a fib/flutter → v fib → asystole
- Treat with rewarming and standard ACLS methods
- Need to be >30ºC for cardioversion
- Pacing: transcutaneous>transvenous
- Renal
- Cold diuresis
- Vasoconstriction (pseudo-volume overload) leads to increased UO
- ADH is decreased
- Decreased secretion
- Decreased tubular sensitivity
- Capillary leak
- Adds to “rewarming shock”
- Consider rhabdo – CPK
- Cold diuresis
- Acid/Base
- PaO2 decreased 7.2% per ºC
- PaCO2 decreases 4.4% per ºC
- pH increases 0.015 per ºC
- “pH stat” – correct pH with CO2; where “alpha stat” has no correction
- Electrolytes are an issue
- K will shift into cells, and will be released with rewarming!
- Coagulopathy
- Plts are sequestered
- Decreased coagulation factors
- ?fibrinolysis
- not significant until <34ºC
- ?fibrinolysis
- #1: ABCs!! and then treat the underlying cause
- “Umbles”
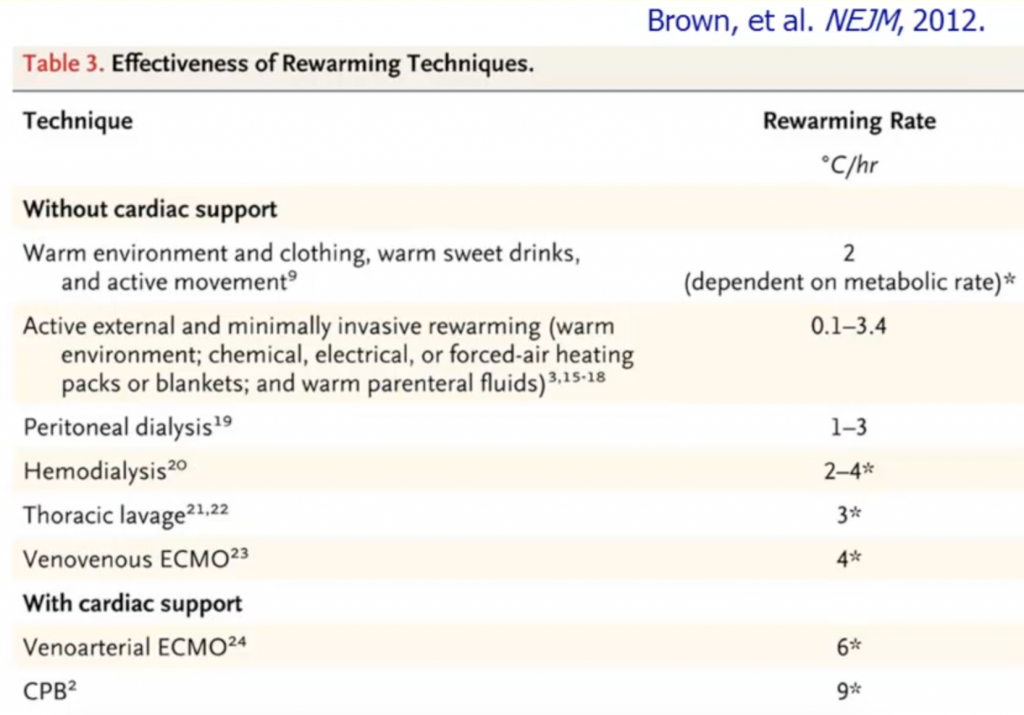
- Re-warming
- Passive external rewarming
- Blanket
- Active external rewarming
- Warm water
- Heating pads
- Heated air convection blankets
- Afterdrop
- As the cold blood from the extremties is shunted to the core and is associated with a drop in temperature
- Active internal rewarming
- Airway rewarming
- Warm IV fluids
- Warm irrigation of pleural, peritoneal, mediastinal spaces
- Esophageal cooling/warming device
- Intravascular device: Servo controlled via central line
- VA-ECMO!
- Passive external rewarming
- Signs of irreversibility
- Injuries incompatible with life
- Hypothermia after prolonged normothermic cardiac arrest
- pH <6.8 or K >12 mEq/L
- Chest wall decompression is impossible
- Miscellaneous factors associated with hypothermia:
- Drowning
- Risks: Male, <20yo, pre-existing conditions (sx do), alcohol, ineffective safety barriers, hyperventilation (Shallow water blackout syndrome)
- Resuscitate if <1 hour
- Inhalation of water (not always)
- Pulm edema
- Aggressive treatment until warm
- Frostbite
- Minimize exposure and additional trauma (no massage)
- Warm water bath (not hot water)
- Debride or amputate
- Wait for demarcation
- Drowning
Hypothermia and trauma
- Predisposed to hypothermia due to:
- Exposure, blood loss, infusion of cold fluids, limited heat production
- Worry about the Triad of Death
- Hypothermia < 35°C = 3x risk of death!
Therapeutic hypothermia
- Populations:
- Cardiac arrest
- Aim for core temp of 32 – 36 °C for at least 24 hours after achieving target temperature
- Head trauma/TBI
- NABISH I: no benefit of hypothermia
- NABISH II: earlier cooling was beneficial for SDH/EDH
- Eurotherm study: hypothermia for elevated ICP after TBI
- No benefit!
- Actually: favored Normothermia
- Spinal cord injury
- Limited data
- Miami project of ASIA A patients cooled + early decompression
- Some people improved
- Miami project of ASIA A patients cooled + early decompression
- Limited data
- CVA
- Ongoing trials, no data yet
- Acute myocardial infarction
- Cooling w/in 6 hrs of STEMI, x 1.3-4.5 hours, with primary PCI
- No benefits
- Cooling w/in 6 hrs of STEMI, x 1.3-4.5 hours, with primary PCI
- Acute hepatic failure
- Decreased ICP
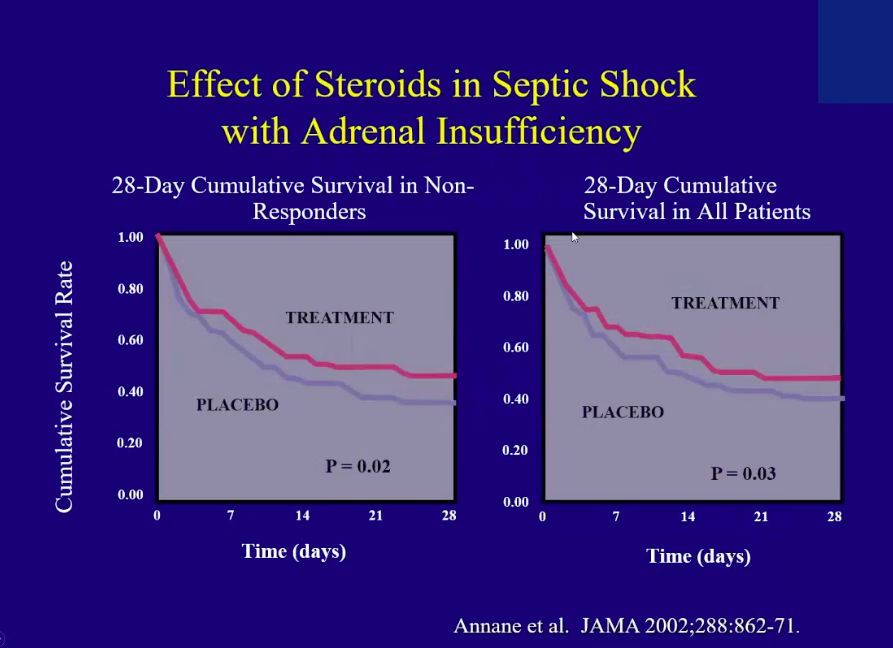
- ARDS/Sepsis
- Ongoing trials, no data yet
- Cardiac arrest
- TTM- How to do it?
- Same mechanisms for rewarming but used to cool
- Treat shivering
- Sedation
- NMB
- Surfaced warming
- Medications while awake!
- High dose Valium
- Precedex gtt
- Emergency preservation and resuscitation (hypothermia for trauma!)
- Animal data: the colder the animal is, the longer they can tolerate an arrest
- Kept cooled x 36 hours = great outcomes
- EPR-CAT Trial
- Need to identify candidates w/in 5 minutes of pulselessness
- 18-65 yo w/ signs of life on hospital arrival
- Cool to 10ºC → hemostasis → CPB/Control bleeding
- End point: survival without significant neuro deficts
- Currently ongoing at STC
- Need to identify candidates w/in 5 minutes of pulselessness
- Animal data: the colder the animal is, the longer they can tolerate an arrest
Suggested Reading
- Lantry J, Dezman Z, Hirshon JM. Pathophysiology, management and complications of hypothermia. Br J Hosp Med (Lond). 2012 Jan;73(1):31-7. [Pubmed Link]
- Brown DJ, Brugger H, Boyd J, Paal P. Accidental hypothermia. N Engl J Med. 2012 Nov 15;367(20):1930-8. [Pubmed Link]
- Donnino MW, Andersen LW, Berg KM, Reynolds JC, Nolan JP, Morley PT, Lang E, Cocchi MN, Xanthos T, Callaway CW, Soar J; ILCOR ALS Task Force. Temperature Management After Cardiac Arrest: An Advisory Statement by the Advanced Life Support Task Force of the International Liaison Committee on Resuscitation and the American Heart Association Emergency Cardiovascular Care Committee and the Council on Cardiopulmonary, Critical Care, Perioperative and Resuscitation. Resuscitation. 2016 Jan;98:97-104. doi: 10.1016/j.resuscitation.2015.09.396. [Pubmed Link]
Podcast: Play in new window | Download
Subscribe: Apple Podcasts | RSS