Today we have the pleasure to welcome Nancy Maureen Hardy, MD, MA, FACP, Associate Professor of Medicine at the University of Maryland Marlene & Stewart Greenebaum Cancer Center. Dr. Hardy originally trained at Duke University for her medical degree, her Internal Medicine residency, and an Oncology fellowship. Next she moved on to the NIH where she completed both an ID fellowship and Research Fellowship in Immunology. She then stayed on the NIH faculty for 10 years at the Experimental Transplantation and Immunology Branch of the National Cancer Institute until 2014. Now we have get genius gracing the halls of UMMC where she acts as the Director of Allogenic Transplantation and Cell Therapy Laboratories. We finally have convinced her to pass along just a small fraction of her genius on what to expect when we see a Stem Cell Transplant patient, a population of individuals that brings chills to the bravest intensivist. Trust me, this is the best way to start the New Year!
Summary assisted by Dr. Ram Baalachandran
Key points:
- Blood and marrow transplantation is used to cure lethal disease
- ICU pts will look bad, but they WILL get better!
- Know the difference:
- Autologous HSCT (hematopoietic stem cell transplantation)
- High dose chemo + stem cell rescue
- Immunological reset in autoimmune diseases/cancer
- <3% transplant-related mortality, usually in-patient, but higher rate of relapse
- Allogenic SCT
- Immunotherapy + graft-vs-leukemia
- Marrow replacement for nonmalignant disease (typical BMT patient)
- 20-40% transplant-related mortality, usually in first 2 years
- Autologous HSCT (hematopoietic stem cell transplantation)
- Never underestimate the potential for quick deterioration!
- Compromised barriers: skin, mucosa
- Immune dysfunction (-penia, immune suppressing drugs, GVHD, autoimmune rxns)
- Treat broadly, narrow when possible
- BE AGGRESSIVE, you will not regret diagnostic procedures/studies
- Timing of complications will influence Ddx and management
- Early/Pre-engraftment: infection vs. drug tox
- Intermediate/Post-engraftment: GVHD vs. infection vs. relapse (bad!)
- Late: GVHD vs. relapse vs. infection (less common)
- Indications of hematopoietic Stem Cell Transplantation (HSCT):
- Autologous transplantation
- Multiple myeloma
- Non-Hodgkin’s lymphoma
- Hodgkin’s disease
- Acute myeloid leukemia
- Autoimmune disorders
- Allogeneic transplantation
- Acute myeloid leukemia
- Acute lymphoblastic leukemia
- Chronic myeloid leukemia
- Myelodysplastic syndromes
- Myeloproliferative disorders
- Non-Hodgkin’s lymphoma
- Hodgkin’s disease
- Chronic lymphocytic leukemia
- Multiple myeloma
- Aplastic anemia
- Sickle cell anemia
- Autologous transplantation
- Procedure:
- Autologous HSCT:
- Mobilization and Leukapheresis of patient stem cells
- Usually collected during recovery after chemotherapy in cancer patients
- Storage with DMSO, liquid Nitrogen
- 24 hours after chemotherapy cells are thawed and infused
- Usually response (increase in WBC) seen in 9 days
- Increase in platelet count seen in 13-14 days
- Mobilization and Leukapheresis of patient stem cells
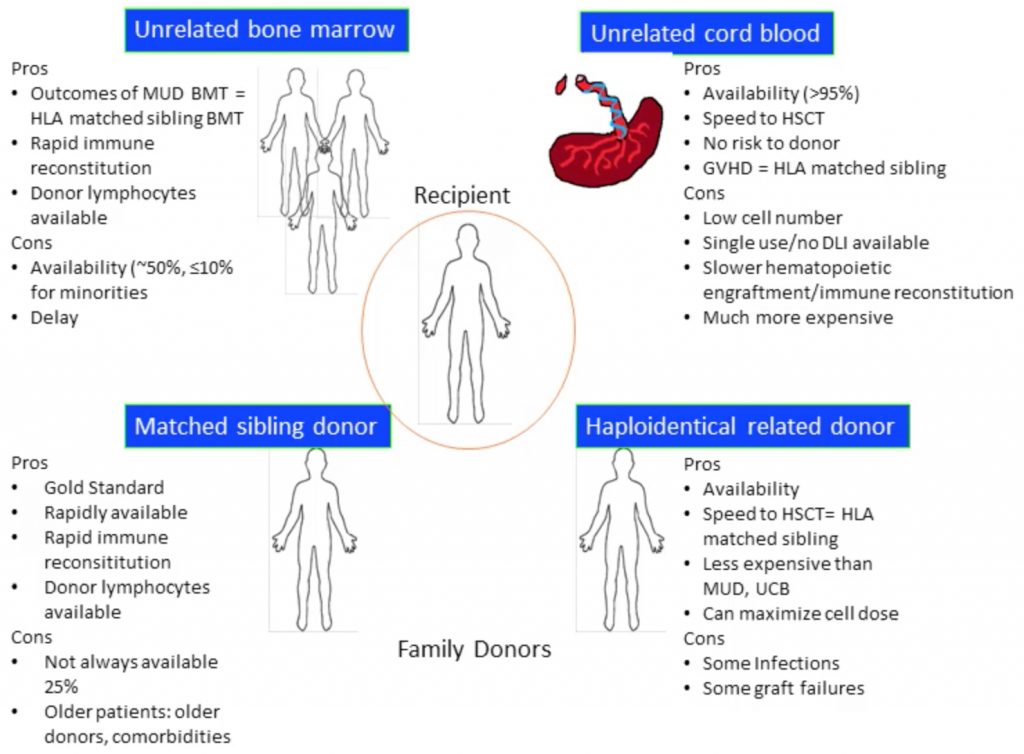
- Allogeneic HSCT:
- Donor collection-> Processing-> cryopreservation-> chemotherapy-> infusion
- Donor options:
- HLA identical sibling: 25%
- Matched unrelated donor
- Cord blood
- Can tolerate mismatch, but low quantity obtained with each collection, and it is expensive
- Mismatched related
- Parent, sibling, or child of a patient with only one identical HLA haplotype
- But associated with increased risk of CMV, BK virus infection and hemorrhagic cystitis
- Donor options:
- Donor collection-> Processing-> cryopreservation-> chemotherapy-> infusion
- Autologous HSCT:
- Complications:
- Acute GVHD and HLA mismatch (risk factors for ICU admission)
- Short- and long-term survival of patients admitted to the ICU remains dismal and depends on the number of organ failures
- Acute GVHD and HLA mismatch (risk factors for ICU admission)
- Risks associated with Mobilization and collection:
- G-CSF given before harvesting can cause splenic rupture
- Important differential diagnosis in patients presenting with abdominal pain
- Central line insertion can be associated with complications like hemorrhage, infection, pneumothorax
- G-CSF given before harvesting can cause splenic rupture
- Risks associated with storage:
- Citrate used for storage can cause hypocalcemia
- Rare complication but potentially life threatening
- Hypervolemia
- Unusual since the volume of infusion is low (180 cc); especially in patients with Amyloidosis
- Anaphylaxis associated with DMSO
- Heparin Induced Thrombocytopenia
- Very low dose of heparin used, thus unusual
- Citrate used for storage can cause hypocalcemia
- Adverse effects of High dose Chemotherapy:
- Cytopenia
- Organ Failure, especially renal failure, can persist for 3 months
- Risks: Engraftment:
- Engraftment syndrome:
- Sudden onset
- More than expected WBC increase in short duration
- Cytokine mediated
- Presents as hypotension, AKI, non-cardiogenic pulmonary edema
- Treatment with steroids
- Immune Reconstitution Inflammatory Syndrome (IRIS)
- Can present with viral pneumonia
- Diffuse Alveolar Hemorrhage
- Factor VIIa used in treatment, can be instilled in endotracheal tube
- Engraftment syndrome:
- Risks: Graft Failure:
- Prolonged aplasia
- Stem cell loss
- Prior treatment
- Processing failure
- Trafficking issue
- C. difficile infection
- Thrombosis (may take 3-4 months for WBC to increase)
- Inherent defect
- It is important to identify complications early, espec ially infection, perform necessary diagnostic procedures and initiate treatment in timely manner
- Outcomes:
- Cause of death in Autologous HSCT:
- 70%- Relapse
- 20% – Infection
- 2% – Organ failure
- 1% – 2nd Malignancy
- Cause of Allogeneic HSCT:
- Most common – 48% – Organ failure
- 2nd most common – 17% – Infection
- Cause of death in Autologous HSCT:
Suggested Reading
- Copelan EA. Hematopoietic stem-cell transplantation. N Engl J Med. 2006 Apr 27;354(17):1813-26. [Pubmed Link]
- Pène F, Aubron C, Azoulay E, Blot F, Thiéry G, Raynard B, Schlemmer B, Nitenberg G, Buzyn A, Arnaud P, Socié G, Mira JP. Outcome of critically ill allogeneic hematopoietic stem-cell transplantation recipients: a reappraisal of indications for organ failure supports. J Clin Oncol. 2006 Feb 1;24(4):643-9. [Pubmed Link]
- Juric MK, Ghimire S, Ogonek J, Weissinger EM, Holler E, van Rood JJ, Oudshoorn M, Dickinson A, Greinix HT. Milestones of Hematopoietic Stem Cell Transplantation – From First Human Studies to Current Developments. Front Immunol. 2016 Nov 9;7:470. [Pubmed Link]
- Benz R, Schanz U, Maggiorini M, Seebach JD, Stussi G. Risk factors for ICU admission and ICU survival after allogeneic hematopoietic SCT. Bone Marrow Transplant. 2014 Jan;49(1):62-5. [Pubmed Link]