Today we at the University of Maryland are honored to host Michael Rothman, Ph.D., co-founder and chief science officer, PeraHealth. Dr. Rothman holds Bachelor and Master of Science degrees in chemistry from Brown University and a Ph.D. in chemistry from the University of Michigan. After losing his mother to an undetected complication following a low-risk surgical procedure, Dr. Rothman was determined to develop a method to predict such travesties before they occurred. He accomplished this by leveraging over 30 years of data analysis and mathematical modeling experience to create a method of tracking patient progress, allowing detection of declining health, and allowing earlier intervention. These models are referred to as the Rothman Index and the pediatric Rothman Index, both of which are revolutionizing the way we care for critically ill patients. I can be assured of very little in life, but I can promise you: this lecture will change the way you practice medicine and WILL save the lives of those around you!
Clinical Pearls (assisted by Lia Losonczy, MD MPH)
Bottom line:
- The Rothman Index is a composite number based on:
- Key nursing assessments
- Vital signs
- Laboratory values
- Helps predict the patient’s risk of death
- The trend of this score helps identify patients who are at high risk of decompensating
- Validated by 24 peer-reviewed articles, 33 conference presentations, and numerous ongoing studies!
- 8300 times cited!
The Rothman Index Model:
- Heart of Model is 3 pronged:
- Nursing Assessment
- All nurses make assessments of patients by system
- These assessments have binary value: either they meet or do not meet the standard for that assessment
- Example: GI system standard requirement would be that the patient has a soft, non tender abdomen, with present bowel sounds present, no nausea or vomiting, no incontinence
- Must ALL to be true that met the standard
- If one is not met, did not meet standard.
- Assessments are recorded at least twice a day
- Example: GI system standard requirement would be that the patient has a soft, non tender abdomen, with present bowel sounds present, no nausea or vomiting, no incontinence
- All hospitals record essentially the same data, but in different ways
- Rothman standardizes the reporting between hospitals so it can be compared
- Early findings:
- Nursing assessments serve as early indicators of decompensation even when patient maintains normal vital signs
- Confusion, dietary changes, development of edema
- Ex: patients are 9.4 times more likely to die in hospital with a failed neuro assessment
- Nursing assessments serve as early indicators of decompensation even when patient maintains normal vital signs
- Estimation of Risk
- Abnormal values of certain lab tests and vital signs predicted risk of mortality
- Using population norm estimates, the Rothman Index is able to identify both normal values and escalation of risk with data trends
- Ie: more deviation from normal leads to an escalation of mortality risk
- Nursing Assessment
- Common Scale (Data Fusion)
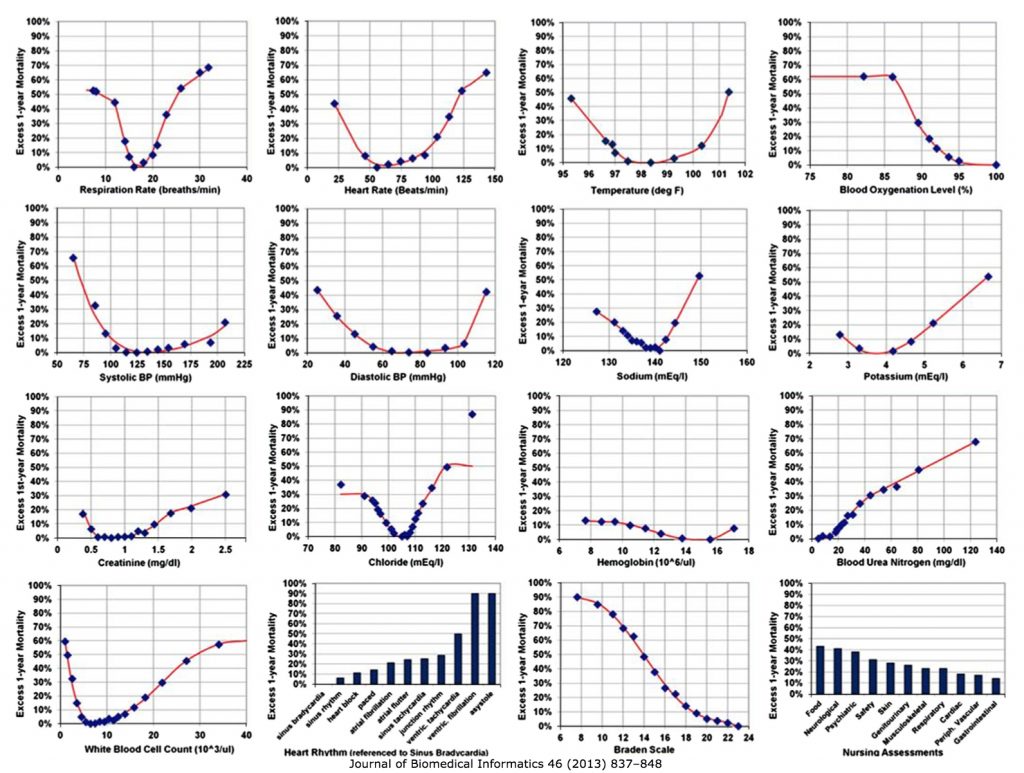
- Each variable in the index can be charted to an excess risk curve (see above)
- Greatest impact: Food/Nutrition
- Created a way to codify each patient’s risk of death from all of these metrics
- Sum risk over total number of variables (26 possible)
- Normal = no risk = 100
- Lower the score, the sicker the patient
- Normal = no risk = 100
- Each variable in the index can be charted to an excess risk curve (see above)
How to use and interpret the Index score:
- This Index was built to capture the concept of risk
- Validated at 3 different hospitals to predict risk of 24 hour mortality
- Better predictor of mortality compared to Apache III
- Has also been validated to predict 30 day risk of readmission
- Correlates with both length of stay and cost of stay
- Validated at 3 different hospitals to predict risk of 24 hour mortality
- Follow trends for predictions:
- Very High Acuity rule
- Has the patient’s score been below 20?
- If yes, mortality risk 25.9% if no, 0.3%
- This rule captures 86% of deaths
- Patients who trigger the Very High Acuity Rule, they are 80 times more likely to expire in the hospital
- If yes, mortality risk 25.9% if no, 0.3%
- Has the patient’s score been below 20?
- High Acuity Rule
- Index falls 50% within 24 hours: risk of mortality is 16.6%
- Medium Acuity Rule
- Index falls 30% within 6 hours: risk of mortality is 10%
- Very High Acuity rule
- Other uses:
- Earlier identify people appropriate for palliative care consult
- Measure current hospital admission score against previous admissions
- Graph a patient’s overall trajectory
- Assist to triage patients who are appropriate to leave the ICU
- Can help predict readmission to an ICU
- Prioritize who should be rounded on/triaged first
- Can decrease mortality by up to 30% in multiple studies, especially related to sepsis!
Overall, can be utilized to prioritize your attention!
Suggested Reading
- Piper GL, Kaplan LJ, Maung AA, Lui FY, Barre K, Davis KA. Using the Rothman index to predict early unplanned surgical intensive care unit readmissions. J Trauma Acute Care Surg. 2014 Jul;77(1):78-82. [Pubmed Link]
- Rothman MJ, Rothman SI, Beals J 4th. Development and validation of a continuous measure of patient condition using the Electronic Medical Record.J Biomed Inform. 2013 Oct;46(5):837-48. [Pubmed Link]
- Finlay GD, Rothman MJ, Smith RA. Measuring the modified early warning score and the Rothman index: advantages of utilizing the electronic medical record in an early warning system. J Hosp Med. 2014 Feb;9(2):116-9. [Pubmed Link]
- Rothman SI, Rothman MJ, Solinger AB. Placing clinical variables on a common linear scale of empirically based risk as a step towards construction of a general patient acuity score from the electronic health record: a modelling study.BMJ Open. 2013 May 14;3(5). [Pubmed Link]