Summary written by Dr. Mustafa Abdulmahdi
General Issues
- Patient at <20 week gestation can be treated similar to other ICU patients
- Fetus <32 week gestation may benefit from magnesium sulfate (less cerebral palsy in pre-term infants)
- Administration of betamethasone upon admission to ICU if you expect delivery in 1-2 weeks is not unreasonable
- After 18-20 weeks gestation, start to see hemodynamic effects in mother
Fetal Heart Rate Categories
- Category 1: Reassuring, 110-160 with variability and accelerations
- Category 2: Between category 1 and 3
- Category 3: Ominous, absent variability (marker of fetal hypoxia/acidosis), late decelerations, bradycardia. Outside the ICU setting, delivery within 30 minutes is indicated.
Pregnancy-Related Respiratory Compromise
- Hypoxia (e.g., PE, flu, pulmonary edema, critical illness)
- Hypercarbia (e.g., excess narcotics, obese/OSA, high spinals, AMS)
- Notoriously difficult airways
- Gastric dysfunction
- Decreased FRC leading to rapid hypoxia
- Poor view due to laryngeal edema (more with eclampsia)
- Increased bleeding risk with airway manipulation
- No RCTs with NIPPV in pregnant patients, but theoretical risk of aspiration, known risk of rapid hypoxia due to decreased FRC
- ARDS (1:6500 deliveries)
- Maternal mortality 9%
- Increased risk of preterm labor with fetal/maternal death
- Fetus sees far less pO2 than Mom, so goal pO2 is >70, O2 sat >95%
- How do you know you are adequately oxygenating the fetus? -> Look at FHR
- Proning, neuromuscular blockage, other modes of ventilation, and recruitment maneuvers have not been studied, but consensus is to do what you are able to
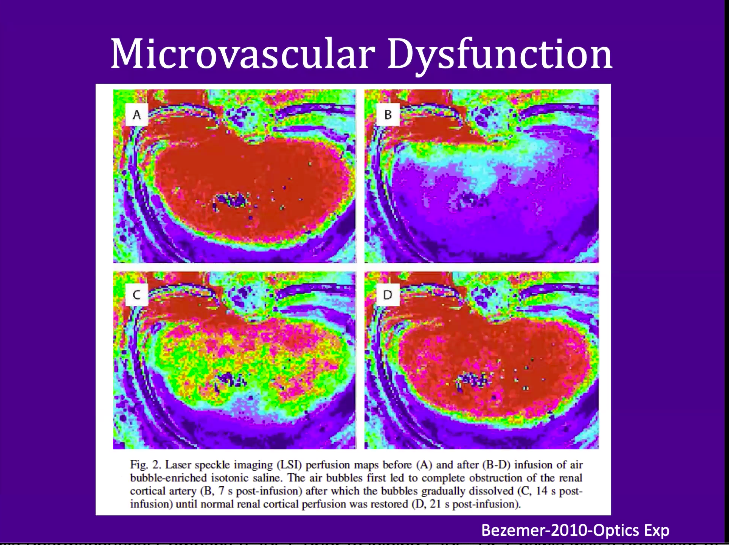
Cardiovascular Compromise
- 20-30% of maternal blood volume goes to the uterus
- With CPR, CO drops to approx 10% (imagine what the fetus is seeing)
- With shock, keep aorto-caval compression in mind
- Regarding pressors, no human models for ureteroplacental blood flow (ephedrine is commonly used)
Preeclampsia/Eclampsia
- 2-8% of all pregnancies
- Eclampsia presents with TONIC/CLONIC seizures (AMS does not equal eclampsia)
- Eclampsia increases risk of ICH, cerebral edema, cerebral thrombosis
- May coincide with HELLP syndrome
- HELLP syndrome generally associated with HYPERtension and normo-glycemia (differentiates from acute fatty liver of pregnancy)
- Administration of magnesium sulfate helps prevent the next seizure (4gm
over 4 minutes with goal levels 4-7)
- Treatment of magnesium toxicity = calcium
- Treatment is delivery of the fetus
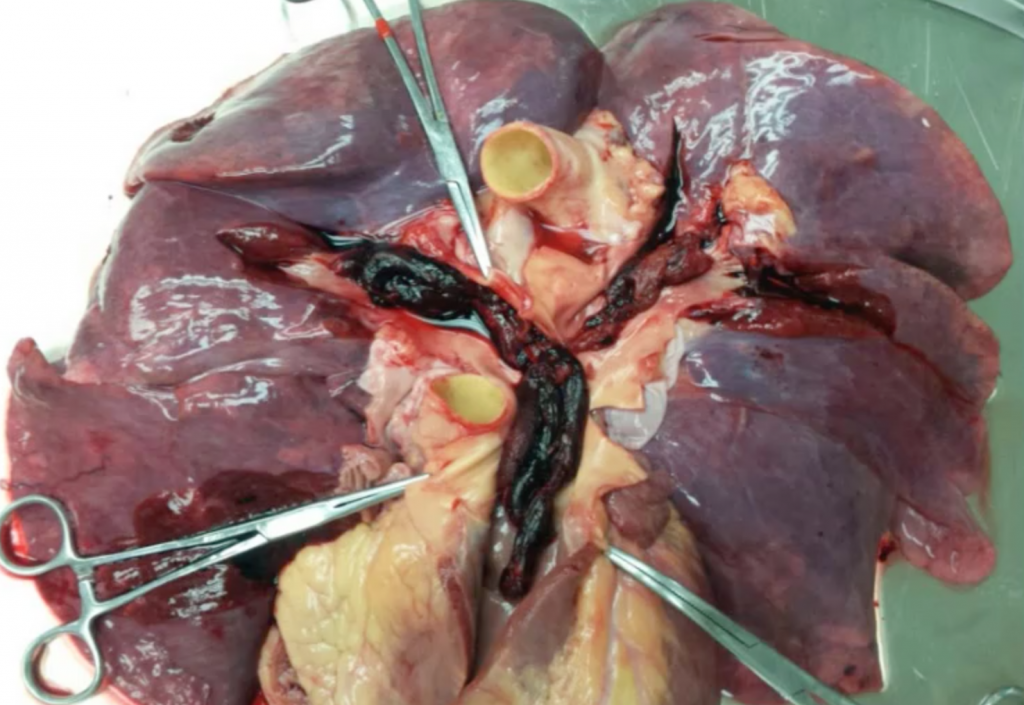
Liver Hemorrhage
- 50% maternal mortality
- SEVERELY elevated transaminases, coagulopathy, RUQ pain
- Initially hypertensive then become hypotensive with shock
Amniotic Fluid Embolism
- 1 in 8,000-80,000 pregnancies
- Cardiogenic/distributive shock picture (LV failure, increased PA/PCWP, massive inflammatory response)
- Hypoxemia secondary to severe V/Q mismatch
- DIC
- 30-40% mortality, however if patient survives the first hour, the mortality drops
- Treatment is supportive care
Acute Fatty Liver of Pregnancy
- 1 in 10,000 pregnancies
- Acute liver failure and encephalopathy without seizure
- Usually hypoglycemic
- Usually normo to hypotensive
- DIC
- Fetus is unable to metabolize long chain fatty acids
- Treatment is delivery of the fetus
Cardiac Arrest Pearls
- Call OB/peds to bedside for potential C-section
- Consider maneuvers such as left uterine displacement
- Consider smaller ETT size due to anticipated difficult airway
- IV access should be above the diaphragm due to aortocaval compression