Welcome back to MCCP! To kick things off we welcome in Dr. Michael Mazzeffi, Associate Professor of Anesthesia at the UMMC, where he additionally acts as the Director for Resident Research Education and Adult Cardiothoracic Fellowship Program Director. He has fast become one of the foremost experts in the field of mechanical circulatory support, publishing numerous papers on the topic. Additionally, his academic prowess has yielded invitations to speak at many prestigious locations around the world. Dr. Mazzeffi was recently a key speaker at the 2016 International Anesthesia Research Society and today he has graciously offered to give us the talk that was the talk of the symposium!
Podcast: Play in new window | Download
Subscribe: Apple Podcasts | RSS
Clinical Pearls (assisted by Jessica Buchner, MD)
Bleeding events on ECMO: Mazzeffi et al.
- 1/2 of all patients have a serious bleeding event while on VV or VA ECMO
- Defined as event that leads to ≥2U PRBC transfusion
- Highest risk in post-cardiotomy shock patients
- VA>VV ECMO
- Overall: 10 events per 100 ECMO days
- Defined as event that leads to ≥2U PRBC transfusion
- Bleeding impacts survival
- ~20% difference in mortality rates
- Predicting who will bleed: HTN, Age>65, ECMO Type (all 3=HAT score)
- Absolute risk of bleeding not as high if platelets >50,000
LVAD patients
- Predominant risk is for GI bleeding, especially with newer non-pulsatile devices
- Harvey et al.: bleeding risk 15-40%
- In addition, LVAD patients are at risk for ICH
- Wilson et al.: ICH risk 30%, possibly related to HTN
- 33% mortality with ICH
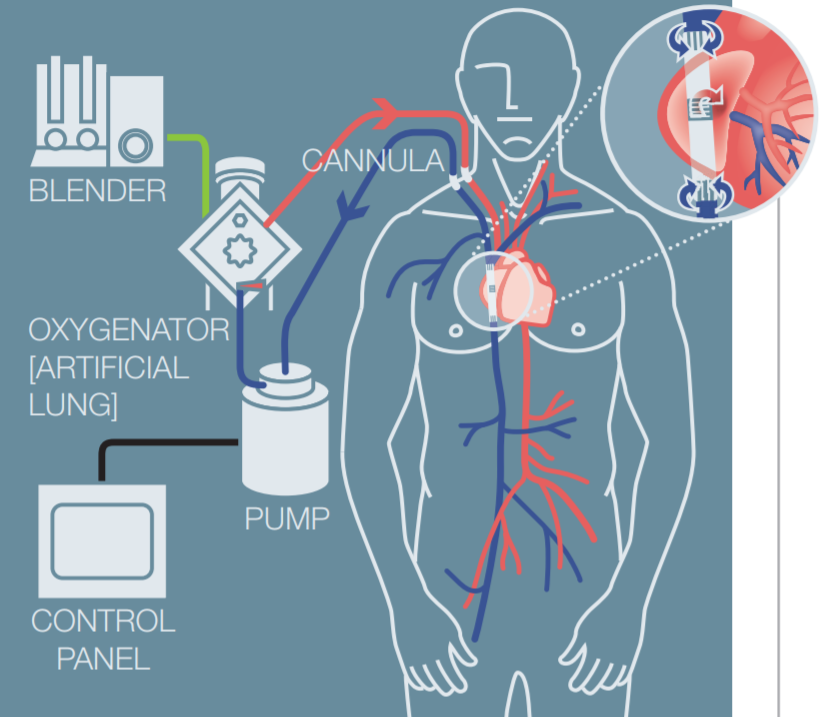
Why do patients on mechanical circulatory support bleed more?
- Shear stress and blood trauma
- 2400 RPM = 5X the normal physiology shear stress
- Change in platelet morphology, not platelet numbers
- More lysis and platelet fragmentation
- Increased platelet activation
- Loss of VWF multimers
- Change in conformation of multimer causing poor platelet adhesiveness
- VWF is stored in endothelial cells & alpha granules of platelets and subendothelial connective tissues
- Alpha 1 domain binds platelets (GP1b), alpha 3 binds collagen
- Change in conformation makes them non-functional
- Makes it easier for ADAMTS13 to cleave multimers, leading to break down
- Type O blood has less vWF at baseline
- ABO type doesn’t make difference in overall bleeding events
- Massive transfusions are more often in the type O group
Coagulation profile is affected on ECMO: Days 1, 3, 5, 7, 12, 16 Nair
- Slight drop to plt count
- Supernormal intrinsic pathway due to up-regulation of factor VIII
- ROTEM
- EXTEM normal to slightly increased
- INTEM mostly normal
How should we anticoagulate?
- ECMO
- High vs low ACT group- Yao
- Significantly higher rates of major bleeding in high group (70% vs 20%)
- No difference in thrombosis rate (high ACT group actually had more thromboses)
- High vs low ACT group- Yao
- LVAD
- Standard is warfarin + aspirin
- Goal INR 1.5-2.5
- Alternative: Dipyridamole (shorter half life)
- Standard is warfarin + aspirin
Management of bleeding
- Hemostatic agents
- DDVAP: 0.3-0.4 ug/kg
- Increases release of endogenous vWF
- No RCTs exist to prove benefit in mechanical circulatory support
- VWF-factor VIII concentrate: 40-80 IU
- Factor VIII has longer half life than vWF (risk thrombosis)
- Expensive
- No RCTS exist to prove benefit in mechanical circulatory support
- Cryoprecipitate
- Exposes the patient to multiple donors and therefore risk for antibody formation (transplants)
- Most device patients also have increased fibrinogen levels
- Platelets
- Optimal count not known
- Uncertain how to monitor
- PFA 100? Platelet mapping?
- Antifibrinolytics
- Data sparse
- One large observational study in pediatric EMCO patients showed decreased bleeding events
- rFVIIa
- 15 patient case series (11 VA ECMO patients, 4 VV ECMO patients)
- Only 1 patient had major stroke
- 15 patient case series (11 VA ECMO patients, 4 VV ECMO patients)
- DDVAP: 0.3-0.4 ug/kg
- Airway Bleeding
- Can use Fogarty balloon or grasper
- IP is critical
- Argon plasma coagulation or cryotherapy for clot removal
- In an RVAD, perhaps too much flow?
- Can use Fogarty balloon or grasper
- Nose bleeds
- Common in VA ECMO
- Continue AC
- Pack with polyvinyl alcohol or oxidized cellulose + wait! (can be weeks)
- Add prophylactic abx and correct thrombocytopenia (if needed)
- Common in VA ECMO
Suggested Reading
- Mazzeffi M, Gupta R, Lonergan T, Pasrija C, Kon Z, Tanaka K. ABO type and bleeding during adult ECMO. Intensive Care Med. 2017 Feb;43(2):275-276. [Pubmed Link]
- Nair P, Hoechter DJ, Buscher H, Venkatesh K, Whittam S, Joseph J, Jansz P. Prospective observational study of hemostatic alterations during adult extracorporeal membrane oxygenation (ECMO) using point-of-care thromboelastometry and platelet aggregometry. J Cardiothorac Vasc Anesth. 2015 Apr;29(2):288-96. [Pubmed Link]
- Kalbhenn J, Schmidt R, Nakamura L, Schelling J, Rosenfelder S, Zieger B. Early diagnosis of acquired von Willebrand Syndrome (AVWS) is elementary for clinical practice in patients treated with ECMO therapy. J Atheroscler Thromb. 2015;22(3):265-71. [Pubmed Link]
- Abrams D, Baldwin MR, Champion M, Agerstrand C, Eisenberger A, Bacchetta M, Brodie D. Thrombocytopenia and extracorporeal membrane oxygenation in adults with acute respiratory failure: a cohort study. Intensive Care Med. 2016 May;42(5):844-52. [Pubmed Link]
- Lonergan T, Herr D, Kon Z, Menaker J, Rector R, Tanaka K, Mazzeffi M. The HAT Score-A Simple Risk Stratification Score for Coagulopathic Bleeding During Adult Extracorporeal Membrane Oxygenation. J Cardiothorac Vasc Anesth. 2016 Sep 1. [Pubmed Link]