Diaphragm Ultrasonography in the ICU
Summary by Dr. Kamel Gharaibeh
Methods to assess diaphragm function
- Transdiaphragmatic pressure (pdi) is the gold standard
- Phrenic stimulation & tracheal occlusion pressure
- CXR
- Fluoroscopy & sniff test
- CT scan
- MRI
- Ultrasound – noninvasive, repeatable, accurate
Of the above modalities, only ultrasound provides information about diaphragm function. Ultrasound provides qualitative & quantitative measures.
Can use both low- & high-frequency probes, depending on what is being measured. When assessing the diaphragm, look for:
- Motion (quiet breathing, voluntary sniffing, & deep breathing)
- Contraction
- Symmetry
- Thickness/atrophy
- Structure
- Injury (e.g., surgery, trauma)
- Adjacent structures or findings
- Measurements (M-mode), including diaphragmatic excursion, thickness, & thickness fraction
Four standard views when assessing diaphragm:
- Subcostal
view:
- Anterolateral approach: anterior axillary line, 7-9th ribs with low-frequency probe directed medially, cephalad, and dorsally towards posterior third of diaphragm
- Mid-clavicular approach: anterior subcostal view with low-frequency probe oriented vertically, below the costal margin along the mid-clavicular line
- Subxiphoid view: low-frequency probe oriented horizontally, directed cephalad, obtaining a cross-sectional view of both diaphragms. Useful for comparing bilateral movement.
- Posterior view needs patient to be sitting up, so may not be feasible in many ICU patients
- M-mode: done with mid-clavicular approach; a waveform is present with each breath
- Zone of apposition, as described below
- Diaphragmatic excursion velocity = a/b, where a is excursion in cm and b is time in sec (normal is 1.3 +/- 0.4 cm/sec, as showed below)
Diaphragm Thickness
- To measure thickness, assess the zone of apposition, which is 0.5-2 cm below costophrenic angle. Usually more easily measured on right side. Use high-frequency probe, 8th-10th ICS, mid-axillary or anterior axillary line, measured at end-expiration (normal thickness 0.22-0.28 cm; atrophy/paralysis usually < 0.2 cm)
- Diaphragm thickening fraction can also be calculated
Clinical Applications
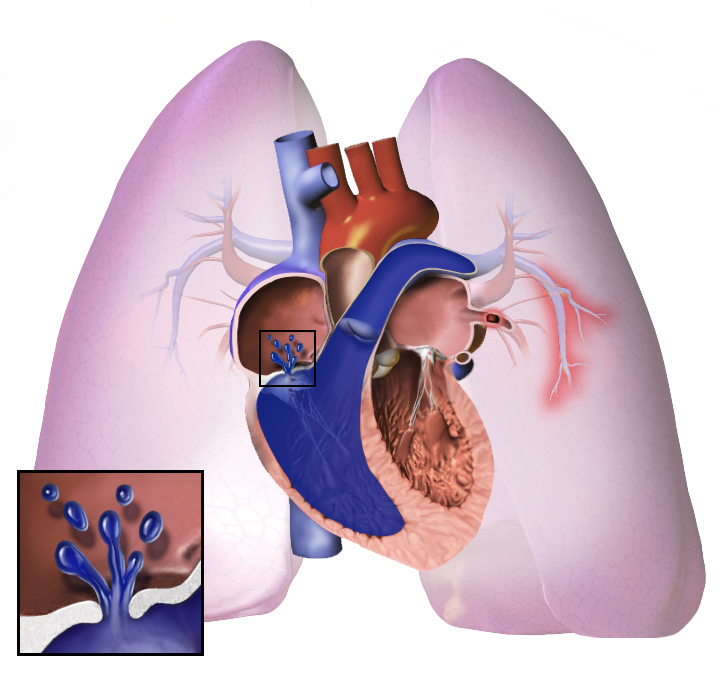
- Ventilator-induced diaphragmatic dysfunction (VIDD)
- Paralysis/Neuropathy
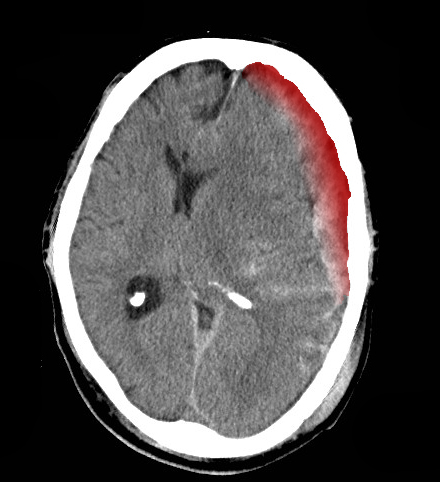
- Paradoxical movement
- Weakness/Myopathy
- Atrophy
- Ventilator weaning
- Vent synchrony
- Intrathoracic pressures
Studies have assessed Diaphragmatic Dysfunction in a variety of clinical scenarios:
- Diagnosing dysfunction or paralysis
- Presence and progression of atrophy
- Assess respiratory workload during MV
- Predict weaning success or failure
Ventilator-induced diaphragmatic dysfunction (VIDD)
- VIDD is common, up to 63% of ICU patients and 2x more common than limb muscle weakness.
- VIDD directly negatively impacts weaning ability and is associated with a poor prognosis (Demoule et al, 2013)
- VIDD onset is usually in first 24 hours
- Changes in diaphragm thickness are common during mechanical ventilation and may be associated with diaphragmatic weakness. Titrating ventilatory support to maintain normal levels of inspiratory effort may prevent VIDD.
- Nutrition in the ICU greatly impacts diaphragm muscle mass. Underweight patients had 43% less diaphragm muscle mass.
We may need to change the mnemonic from “WEANS NOW” to “WEANS DOWN” to include diaphragmatic function….
WEANS DOWN
- W: Wakefulness or sedation reversed
- E: Electrolytes
- A: Acid base balance
- N: Neurologic state
- S: Secretions minimal, cough adequate
- D: Diaphragmatic function
- O: Oxygenation
- W: Work of breathing
- N: Nutrition status
Ultrasonographic measures of diaphragm thickening in the zone of apposition may predict extubation success or failure during SB or PS trials. (DiNino, et al, Thorax 2014)
References
- Sarwal A, Walker FO, Cartwright MS Neuromuscular ultrasound for evaluation of the diaphragm. Muscle Nerve. 2013
- Boussuges A, Gole Y, Blanc P. Diaphragmatic motion studied by m-mode ultrasonography: methods, reproducibility, and normal values Chest. 2009
- Jaber S, Jung B, Matecki S, Petrof BJ. Clinical review: ventilator-induced diaphragmatic dysfunction–human studies confirm animal model findings. Crit Care. 2011
- Demoule A, Jung B, Prodanovic H, Molinari N, Chanques G, Coirault C, Matecki S, Duguet A, Similowski T, Jaber S. Diaphragm dysfunction on admission to the intensive care unit. Prevalence, risk factors, and prognostic impact-a prospective study. Am J Respir Crit Care Med. 2013
- Dres M, Dubé BP, Mayaux J, Delemazure J, Reuter D, Brochard L, Similowski T, Demoule A. Coexistence and Impact of Limb Muscle and Diaphragm Weakness at Time of Liberation from Mechanical Ventilation in Medical Intensive Care Unit Patients. Am J Respir Crit Care Med. 2017
- Goligher EC, Fan E, Herridge MS, Murray A, Vorona S, Brace D, Rittayamai N, Lanys A, Tomlinson G, Singh JM, Bolz SS, Rubenfeld GD, Kavanagh BP, Brochard LJ, Ferguson ND. Evolution of Diaphragm Thickness during Mechanical Ventilation. Impact of Inspiratory Effort. Am J Respir Crit Care Med. 2015
- Ernest DiNino, Eric J Gartman, Jigme M Sethi, F Dennis McCool. Diaphragm ultrasound as a predictor of successful extubation from mechanical ventilation. Thorax Journal 2014