Today we welcome Mojdeh Saba Heavner, Pharm.D., BCPS, BCCCP. Dr. Heavner is an assistant professor here at the University of Maryland School of Pharmacy and a clinical pharmacy specialist in the UMMC MICU. She recently came back to us after a Critical Care & Transplant Specialty Pharmacy Residency at Yale, where she was voted the BEST Pharmacist in Connecticut. Now she is shaking things up here on MICU daily rounds and has revolutionized the care of our patients. So if you want to avoid the brow beating from your own pharmacist every morning, I highly suggest you listen to this lecture twice!!
Podcast: Play in new window | Download
Subscribe: Apple Podcasts | RSS
Clinical Pearls (assisted by Dr. Mustafa Abdulmahdi)
- Key terminologies:
- Pharmacokinetics (PK)
- Processes conducted by the body on the drug
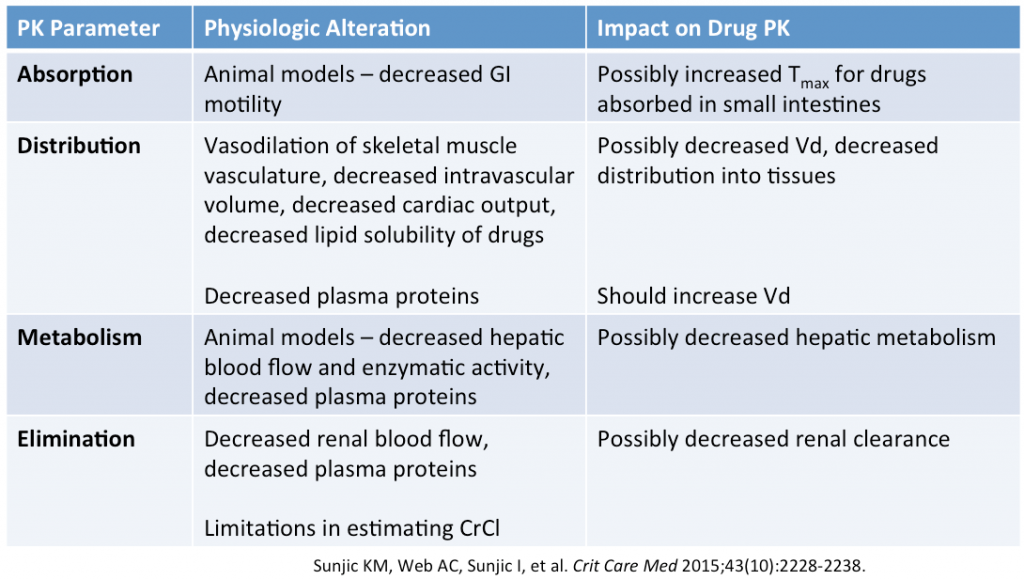
- ADME: Absorption, Distribution, Metabolism, Elimination
- Pharmacodynamics (PD)
- Pharmacologic response resulting from drug at site of action
- Pharmacogenomics
- Pt specific differences in PKPD through genetic polymorphisms
- Pharmacokinetics (PK)
- Absorption: rate & extent that medication enters circulatory system from site of administration
- Rate
- Time to peak concentration (Tmax)
- Impacted by size, solubility, lipophilicity, ionization, and dissociation rate constant of drug
- Time to peak concentration (Tmax)
- Extent
- AUC of the drug
- Bioavailability: fraction of drug that reaches systemic circulation
- ICU concerns
- GI absorption:
- Site
- Stomach: slow absorption, favors acidic drugs
- Small intestine: fast absorption, favors basic drugs (vast majority of ICU drug)
- Considerations in critically ill patients
- Potentially decreased GI absorption due to shunting of blood to vital organs
- Vasopressors might affect GI absorption (controversial)
- Delayed gastric emptying
- Direct interactions of both feeding tube and enteral nutrition with medications
- Site
- Subcutaneous absorption:
- Enoxaparin absorption is altered in ICU patients, especially with increased edema
- Altered PK may lead to sub-therapeutic plasma anti-Xa activity
- GI absorption:
- Rate
- Distribution:
- Volume of distribution (Vd) = relationship between dose & serum concentration
- Factors that affect Vd:
- Lipophilicity increases tissue distribution
- Regional tissue hypoperfusion
- Fluid resuscitation (mainly for hydrophilic drugs)
- Capillary leak/third spacing of total body water (mainly for hydrophilic drugs)
- Plasma protein binding
- Changes in albumin (tend to decrease in critical illness) & alpha-1 acid glycoprotein (tend to increase in critical illness)
- Vd depends on which medication binds to which protein
- e.g., free phenytoin levels increase in critically ill pts with low albumin
- Factors that affect Vd:
- Volume of distribution (Vd) = relationship between dose & serum concentration
- Metabolism:
- Predominant site is the Liver
- Factors in critical illness:
- Serum protein concentrations (changes the free portion of the drug)
- Hepatic enzyme activity (both phase I and II)
- Hepatic flow (Q)
- Hepatic extraction (Eh) of the drug
- Hepatic clearance is dependent on hepatic blood flow and extraction ratio
- (Clh) = Q x Eh → etc
- Fentanyl’s high Eh makes its metabolism highly dependent on Q
- In BRAIN-ICU study, 2 factors impacting fentanyl PK are ESLD & CHF (both diseases affect Q)
- Elimination:
- Predominant site is the Kidney
- Proportional to GFR
- Alteration in critical illness
- AKI
- Hydrophilic medications
- Loading dose (25-50% greater than normal)
- Normal or near-normal maintenance doses
- Practical recommendations
- Monitor serum creatinine and UO trends
- Err on the “more aggressive” approach with abx
- Normal loading doses (increased Vd)
- Round up CrCl to the next higher abx frequency
- Therapeutic monitoring when able
- Hydrophilic medications
- Augmented renal clearance (ARC)
- Increased GFR with possible changes to tubular secretion and absorption
- No standard definition, need urine creatinine collection
- Peaks on ICU 4-5, normalizing by day 7
- ICU factors:
- Increased CO
- Increased Preload
- Risk factors
- Age ≤ 50, trauma, SOFA ≤ 4
- AKI
- Predominant site is the Kidney
Organ support in the ICU and impact on PKPD
- CRRT
- Compared with IHD, CRRT provides a more predictable & constant clearance
- Complicating factors
- ICU pt with AKI are dynamic
- Dialysate/UF flow rates
- Permeability of hemodiafilter
- Age of hemodiafilter (72-96 hrs?)
- Pre- vs. Post replacement solution proportions
- CVVH > CVVHDF > CVVHD
- What affects drug (e.g., abx) clearance in renal replacement therapy?
- Molecular weight
- Vd
- Protein binding
- FDA-approved dose in package insert
- Antimicrobial activity
- e.g., peak concentration, time over MIC, or AUC:MIC
- Dosing weight (Ideal? Actual? Adjusted?)
- MARS:
- Removes minimally dialyzable, lipophilic, albumin-bound molecules + water-soluble molecules removed with CRRT
- No good data on medication dosing
- Case reports only
- ECMO:
- We don’t have good quality data
- Circuit factors
- Tubing, oxygenator, priming fluid type, circuit age
- Sequestering of lipophilic + high protein-bound drugs in the circuit and oxygenator
- Tubing, oxygenator, priming fluid type, circuit age
- Severely ill patients with multiple factors (AKI, TBW, hepatic dysfunction, acid-base, etc.)
- Plasmapheresis:
- Removes 40-60 mL plasma/kg over 2-3 hours
- No good data on clearance
- Drugs likely removed → low Vd (<0.2 L/kg) & highly protein-bound (>80%)
- TTM/Hypothermia:
Suggested Reading
- Hobbs AL, Shea KM, Roberts KM, Daley MJ. Implications of Augmented Renal Clearance on Drug Dosing in Critically Ill Patients: A Focus on Antibiotics. Pharmacotherapy. 2015 Nov;35(11):1063-75. [Pubmed Link]
- Smith BS, Yogaratnam D, Levasseur-Franklin KE, Forni A, Fong J. Introduction to drug pharmacokinetics in the critically ill patient. Chest. 2012 May;141(5):1327-36. [Pubmed Link]