Today we are immensely honored to welcome Timothy G. Buchman, PhD, MD, FACS, FCCP, MCCM, Professor of Surgery and Anesthesiology, Emory University School of Medicine. In addition, Dr. Buchman has served as president of nearly EVERY major critical care society, has published 231 peer reviewed journals, and most recently acts as the Editor in Chief for Critical Care Medicine. In 2012 Dr. Buchman founded the Emory Critical Care Center (ECCC), and as director he has united the care of all the critically ill patients in the Emory Health Care System. In 2014, he directed his focus to the development of the Emory Electronic ICU (eICU), a mecca of telemedicine which has revolutionized the way critical care is administered. Today he is gracious to have flown up in order to speak with us on a very hot topic: where is critical care going and how can we not be left behind?
Clinical Pearls– Assisted by Dr. Tony Basel
- “Change is the only constant”
- 50-60 years ago: upright patients + lots of nurses and no doctors
- 1958: Peter Safar (of Baltimore City Hospital) proposed senior physicians (i.e. intensivists) should staff ICUs
- Manpower: what are the nation’s physician manpower needs?
- Conventional wisdom of 1990-2000 (especially managed care) said “we have too many MDs”
- Pronovost, JAMA 2002, proposed change: “An intensivist in every ICU”
- Angus JAMA: “Can we meet the requirements of an aging population?” then HRSA 2006 confirmed there is an MD shortfall
- PrOMIS conference was held in 2007 showing that “some critical care services will be provided by non-critical-care-boarded-physicians”
- What about APPs?
- CHEST 1991: concluded that properly trained physician extenders could work in ICUs with no increase in adverse events
- 2008 CCM article shows that midlevel numbers continue to rise
- Meanwhile, ICU fellowships were going unfilled (and some continue to go unfilled)
- CHEST 1991: concluded that properly trained physician extenders could work in ICUs with no increase in adverse events
- Currently estimated ~10k practicing, board certified intensivists
- Versus the estimated numbers of APPs in critical care = 2600 PAs + 7150 NPs
- So the number of doctors and APPs are nearly equal
- The time to develop competency may be key (takes 2/3 less time to be an APP)
- How short are we?
- View 1: Leapfrog – very short depending where you are in the US (some better staffed than others) (i.e: numbers are good, just not distributed well)
- View 2: ICUs are full of patients that don’t need to be there, so we may not really be that short (i.e.: we don’t need more ICU doctors because there are few real ICU patients)
- View 3: The workforce has responded; the production number is increasing considerably so we don’t know what it will look like in a few years (i.e.: be patient, the doctors are coming… just stuck in training)
- Technology: CCM 2004 – remote critical care
- Mid-1970s: Cleveland, OH conducted a small study and concluded that they could provide medical care remotely
- Today, there are about 50 eICU programs in the USA
- Cover around 15.5% of ICU beds
- What are we really doing with the eICU?
- Trying to detect and track problems → just providing coverage during “off” hours
- JAMA 2011: better mortality and LOS with eICU
- Cost effectiveness
- Fairly expensive to start (Yoo 2016)
- Have to evaluate per-case revenue and per-case cost to see cost savings → it does take time (Lilly 2017)
- Sidebar on relational coordination
- Between the APPs and teleICU, now re-engineering the social relationships in the ICU
- Emory ICU with doctors/nurses in teleICU with APPs at bedside
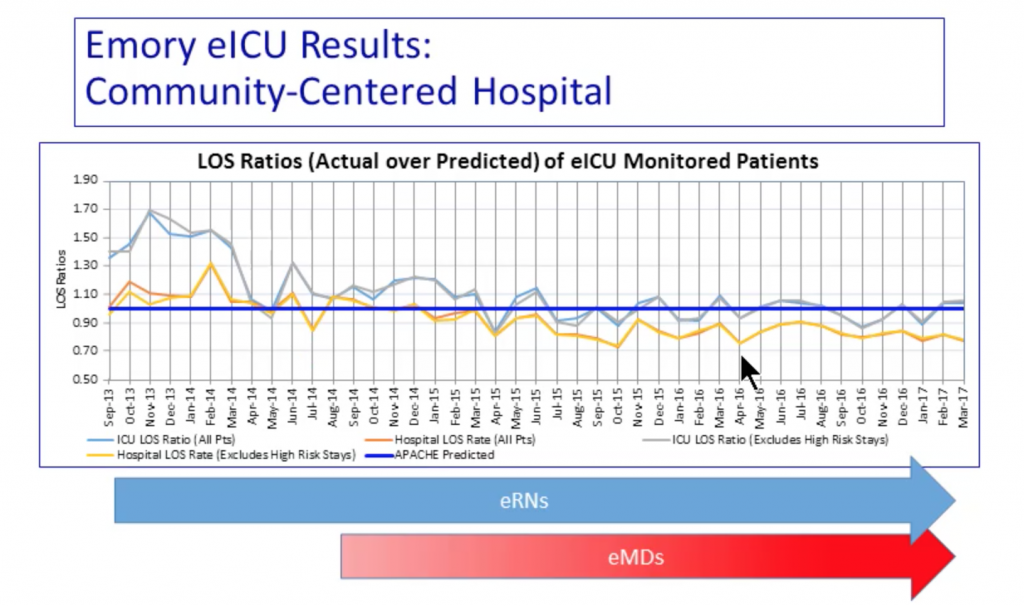
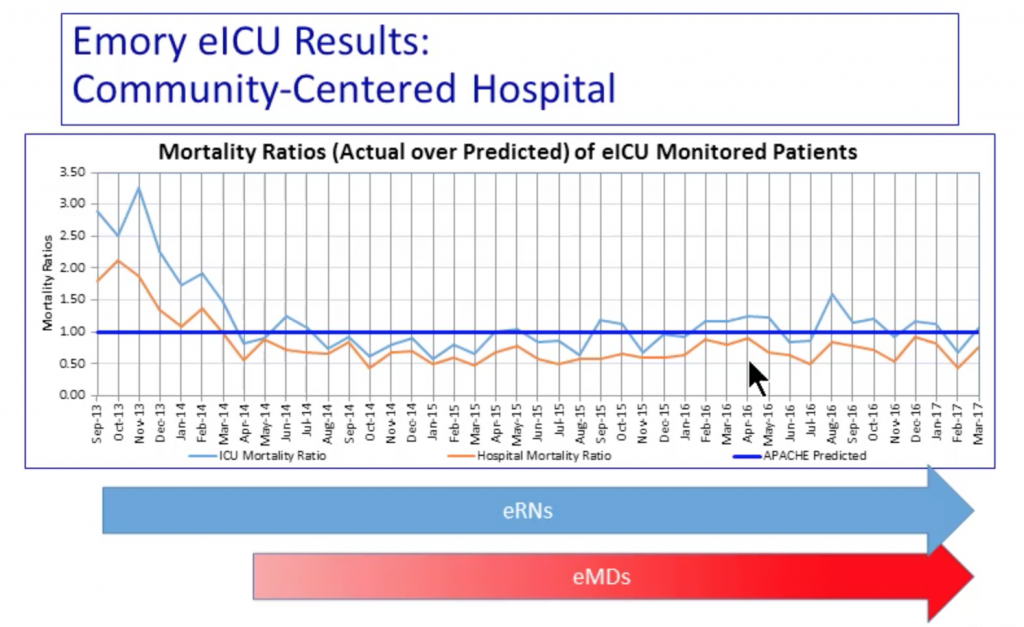
- LOS (both ICU and hospital) improved (saved ~21k ICU days!)
- ICU mortality also improved (Ratio dropped below 1.0)
- Day/Night teams
- Traveling around the world: cover overnight shifts while working in local daylight hours (Australia vs. USA)
- Better for clinicians → shift work has multiple health risks
- Better for patients→ nights tend to be the most “active” times
- Training for teamwork and focus on communication
- Traveling around the world: cover overnight shifts while working in local daylight hours (Australia vs. USA)
- Technology: Mica Endley’s situational awareness
- Situational awareness requires perception, comprehension, and projection
- At bedside: information for “next best decision” + someone with the big picture for “population management”
- We need an EMR with one screen with all the data in one screen in the same place every time → we’re not yet at that level of simplification
- Situational awareness requires perception, comprehension, and projection
- Putting it all together
- Tech is refining and redefining how we approach our tasks
- High risk situations demand high-reliability approaches
- High-reliability approaches need not have all participants co-located; the division of labor may favor that the participants be separated in space (but not in time)
- The 4 Vs of data
- Volume: LOTS of data
- Velocity: coming at a high rate
- Variety: in many forms
- Veracity: data in doubt
- And possibly a 5th: Value
Suggested Reading
- Zehnbauer BA, Buchman TG. Precision Diagnosis Is a Team Sport. J Mol Diagn. 2016 Jan;18(1):1-2. [Pubmed Link]
- Belard A, Buchman T, Forsberg J, Potter BK, Dente CJ, Kirk A, Elster E. Precision diagnosis: a view of the clinical decision support systems (CDSS) landscape through the lens of critical care. J Clin Monit Comput. 2017 Apr;31(2):261-271. [Pubmed Link]
- Buchman TG, Billiar TR, Elster E, Kirk AD, Rimawi RH, Vodovotz Y, Zehnbauer BA. Precision Medicine for Critical Illness and Injury. Crit Care Med. 2016 Sep;44(9):1635-8. [Pubmed Link]
- Buchman TG. A Glimpse of Precision Medicine for Multiple-Organ Dysfunction Syndrome. Crit Care Med. 2016 Nov;44(11):2121-2122. [Pubmed Link]
- Buchman TG, Coopersmith CM, Meissen HW, Grabenkort WR, Bakshi V, Hiddleson CA, Gregg SR. Innovative Interdisciplinary Strategies to Address the Intensivist Shortage. Crit Care Med. 2017 Feb;45(2):298-304. [Pubmed Link]