Today we welcome back one of our favorite graduates of the EM/IM/CCM residency/fellowship here at University of Maryland, Michael C. Scott, MD. Luckily he stayed local and has been paving his own path across town at St. Agnes Hospital of Baltimore, Maryland. Dr. Scott originally hails from San Antonio Texas, where he graduated from the University of Texas Medical School Medical School before heading up to the North East. Since his arrival to Baltimore, Mike has demonstrated a wide knowledge of modern academic literature and has continued to challenge the status quo in medicine! Dr. Scott has proved time and time again that there are no definitives in medicine and today he tackles a very polarizing topic: what to do with a submassive PE?
Podcast: Play in new window | Download
Subscribe: Apple Podcasts | RSS
Clinical Pearls (Thanks to Dr. Ali Tabatabai for assistance with the summary)
- Where is the evidence?
- No good evidence for Surgical or Endovascular Embolectomy for submassive PE at this time.
- No large robust randomized controlled trials for submassive PE in general.
- Guidelines are thus non-existent, treatment not standardized.
- Definitions:
- Massive PE- hemodynamic instability.
- Submassive PE- hemodynamically stable, with some RV dysfunction/strain:
- Elevated Troponin or BNP.
- TTE or CT evidence for RV dilation.
- TTE evidence for RV systolic dysfunction or pHTN.
- Low risk PE- none of the above
- Why do we lyse with thrombolytics?
- Avoid pulmonary HTN and RHF.
- Little data on these actual risks.
- Guidelines:
- ACEP- no data to make a recommendation.
- AHA- can consider is decompensating OR higher risk.
- ESC, ACCP- recommend NOT using thrombolytics unless decompensating to massive PE
- High bleeding risk; based on 2015 meta-analyses.
- Short term mortality benefit was 2.5% vs 3.5% in AC only (statistically significant).
- However, markedly higher rate on major bleed (such as ICH) in PE patients vs trials for MI patients.
- Not due to lack of efficacy; but did note the high number needed to treat.
- High bleeding risk; based on 2015 meta-analyses.
- Avoid pulmonary HTN and RHF.
- How do we risk stratify?
- We want to know who is likely to decompensate!
- Risk scores:
- PESI/sPESI/msPESI
- Low risk scoring that has high sensitivity, but not specific.
- Best used to determine who can be sent home.
- ESC
- Imaging of RV strain +/- lab evidence of RV strain:
- One: low risk.
- Both: moderate/high risk of decompensation.
- Not able to be validated.
- Imaging of RV strain +/- lab evidence of RV strain:
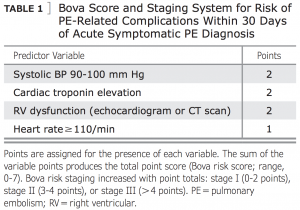
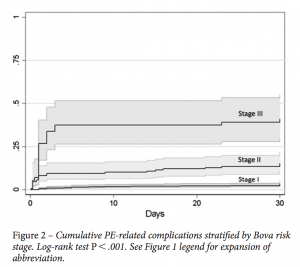
- BOVA
- Defines a stepwise increase in short term risk:
- PESI/sPESI/msPESI
-
-
-
- Sens 26%, Spec 97%, PPV 42%, NPV 93%, PLR 7.93, NLR 0.76
-
-
- Safer alternatives?
- Surgical and endovascular not being discussed as more data needed in comparison to heparin AC alone.
- Likely safer in terms of bleeding risks.
- Catheter-directed thrombolysis
- ULTIMA trial a 2014, the only RCT, a total of 59 pts.
- Submassive defined as RV:LV ratio ≥ 1 on TTE.
- Primary endpoint of improvement of RV:LV ratio at 24 hours.
- However, unclear correlation to risk of hemodynamic decompensation.
- Primary endpoint of improvement of RV:LV ratio at 24 hours.
- Results:
- No difference at 90 days.
- No episodes of hemodynamic decompensation or recurrent VTE in either arm.
- However, appears to be safe.
- Submassive defined as RV:LV ratio ≥ 1 on TTE.
- ULTIMA trial a 2014, the only RCT, a total of 59 pts.
- Half-dose thrombolysis
- MOPETT a 2013 trial (the only RCT)
- Radiographic diagnosis of intermediate risk based on # of lobes involved
- Many patients had lab or imaging evidence of RV strain but was not an inclusion criterion
- Treatments:
- 50kg:
- 10mg bolus, then 40mg over 2 hours.
- <50 kg:
- 0.5mg/kg with a 10mg bolus first, then rest over 2 hours.
- 50kg:
- Primary endpoints: pHTN (PAP ≥40mmHg on TTE) OR pHTN + PE.
- Statistically significant improvement for both in treatment arm
- However, without a right heart cath, the calculated PAP is suspect to some variability and error!
- No episodes of bleeding in either arm
- Mortality numbers similar to other cohorts
- Improvement in PAP persisted at 48 hours, 6 months, and 28 (+/-5) months
- Statistically significant improvement for both in treatment arm
- Radiographic diagnosis of intermediate risk based on # of lobes involved
- MOPETT a 2013 trial (the only RCT)
- Existing data show both catheter-directed and half-dose are safe, but efficacy data are limited
- Surgical and endovascular not being discussed as more data needed in comparison to heparin AC alone.
- Take Home Points:
- Guidelines recommend against routine use of thrombolytics for submassive PE.
- Identifying a higher risk patient group may change risk-benefit balance in favor of thrombolysis.
- Lower risk therapies (e.g., CDT or half-dose thrombolysis) may also change this balance.
- Frank discussion and shared decision making with patients is important.
- Guidelines recommend against routine use of thrombolytics for submassive PE.
Suggested Reading
- Sharifi M, Bay C, Skrocki L, Rahimi F, Mehdipour M; “MOPETT” Investigators. Moderate pulmonary embolism treated with thrombolysis (from the “MOPETT” Trial). Am J Cardiol. 2013 Jan 15;111(2):273-7. [Pubmed Link]
- HKucher N, Boekstegers P, Müller OJ, Kupatt C, Beyer-Westendorf J, Heitzer T, Tebbe U, Horstkotte J, Müller R, Blessing E, Greif M, Lange P, Hoffmann RT, Werth S, Barmeyer A, Härtel D, Grünwald H, Empen K, Baumgartner I. Randomized, controlled trial of ultrasound-assisted catheter-directed thrombolysis for acute intermediate-risk pulmonary embolism. Circulation. 2014 Jan 28;129(4):479-86. [Pubmed Link]
- CChatterjee S, Chakraborty A, Weinberg I, Kadakia M, Wilensky RL, Sardar P, Kumbhani DJ, Mukherjee D, Jaff MR, Giri J. Thrombolysis for pulmonary embolism and risk of all-cause mortality, major bleeding, and intracranial hemorrhage: a meta-analysis. JAMA. 2014 Jun 18;311(23):2414-21.
[Pubmed Link] - Cho JH, Kutti Sridharan G, Kim SH, Kaw R, Abburi T, Irfan A, Kocheril AG. Right ventricular dysfunction as an echocardiographic prognostic factor in hemodynamically stable patients with acute pulmonary embolism: a meta-analysis. BMC Cardiovascular Disorders 2014, 14:64. [Pubmed Link]