Please join me in welcoming Carl B. Shanholtz, MD, Professor of Medicine and Director of the MICU here at the University of Maryland Medical Center. From humble beginnings as a member of the US Navy, Dr. Shanholtz started his medical career in San Diego before finishing his internal medicine here at the UMMC. After graduation he captured an opportunity to be Roy Brower’s clinical research colleague during his Critical Care fellowship at Johns Hopkins University. Since that time he has become a world renowned expert in the field of critical care, possessing well over 100 peer reviewed journals. As the medical director of the UMMC Department of Respiratory Care coupled with 20+ years of research on the topic of respiratory failure (including extensive time spent as an ARDSnet investigator) we could not find a more knowledgable and educated individual to discuss a very sensitive topic: fluid use in the ICU and its overall effect. I assure you, this talk will truly open your mind into exactly how LITTLE we know about fluid resuscitation!
Podcast: Play in new window | Download
Subscribe: Apple Podcasts | RSS
Clinical Pearls
- Why do critically ill patients become volume overloaded?
- Inflammation
- Sepsis
- Pancreatitis
- Trauma
- Burns
- CHF
- Renal Failure
- Inflammation
- Origins of Fluid Resuscitation
- 1830: fluid resuscitation began with the European cholera epidemic
- 1832: first successful saline fluid resuscitation
- 1834: first use of albumin
- 1903: sphygmomanometer invented; shock defined by Mummary and Crile as inadequate BP, with IV saline as one of few treatments
- 1934: Blalock differentiated shock based on circulatory pathophysiology
- Septic shock vasodilatory and hyperdynamic
- Shock “a decrease in the ratio of the blood volume in circulation to the capacity of the vascular tree” (loss of effective blood volume)
- So why give fluids?
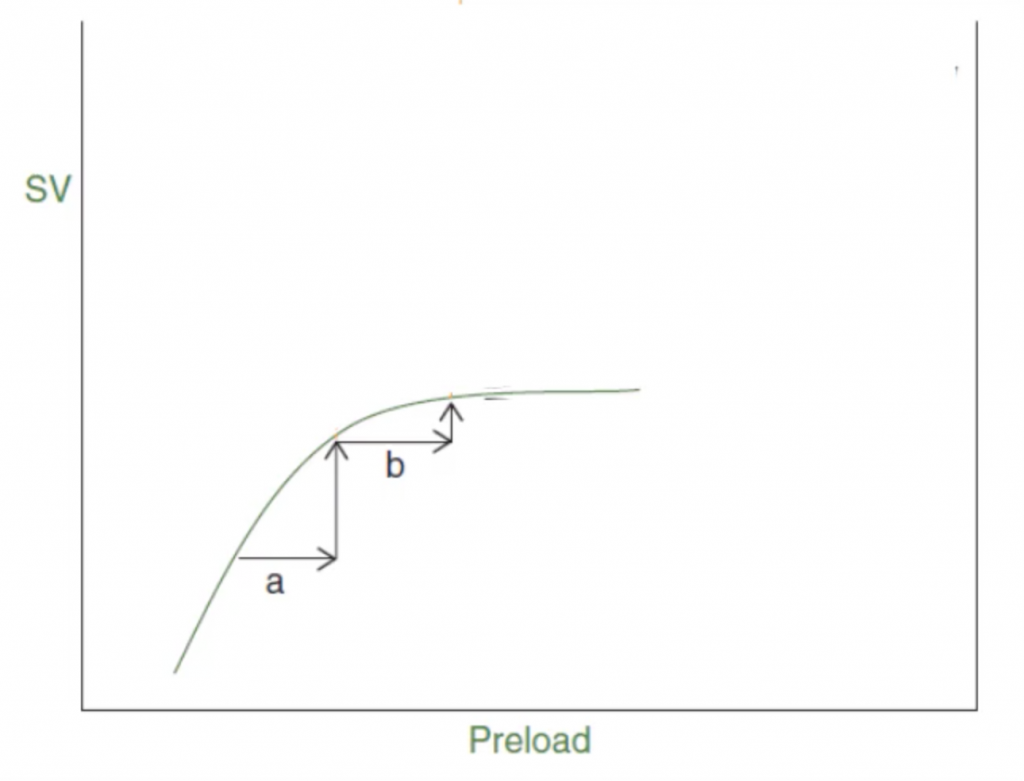
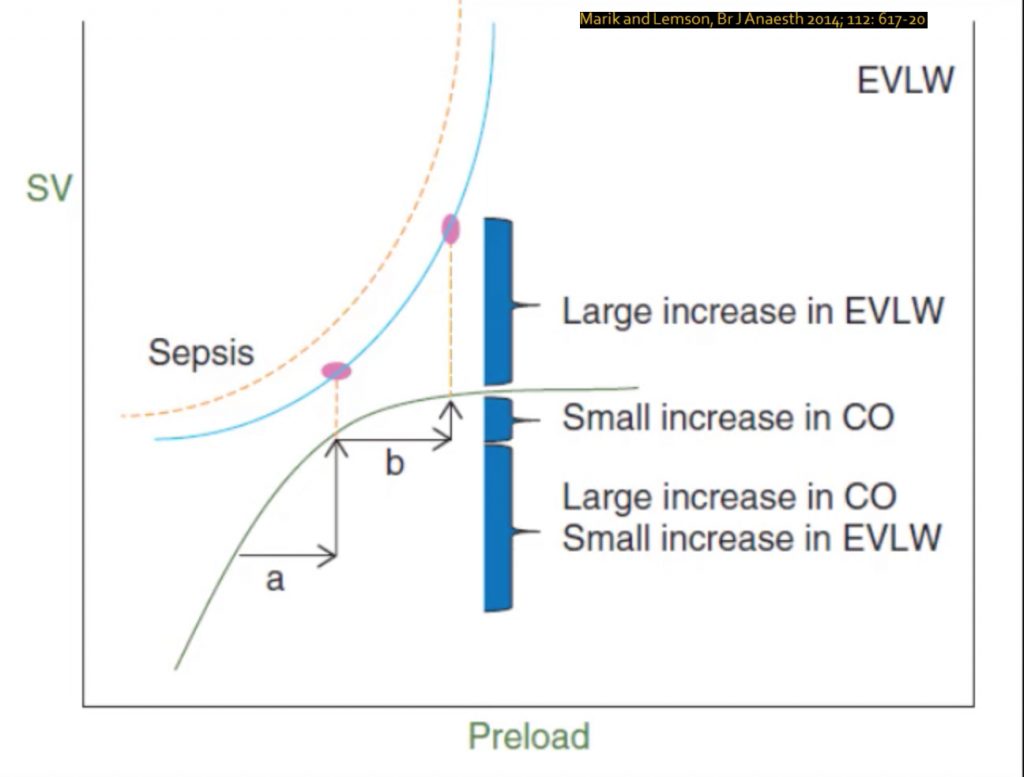
- Frank-Starling curve
- Successive increases the preload by filling the unstressed portions of the heart → increases in SV
- Frank-Starling curve
-
-
- Where in that “a” is volume responsive.
- However, as you continue to increase the preload, the gain to SV diminishes at “b” leading to an unresponsive state.
- Seymour, NEJM, 2017
- Analysis of NY state sepsis data
- Found a 4% increase in mortality for ever hour beyond the first 3 hours of the sepsis bundle
- Analysis of NY state sepsis data
-
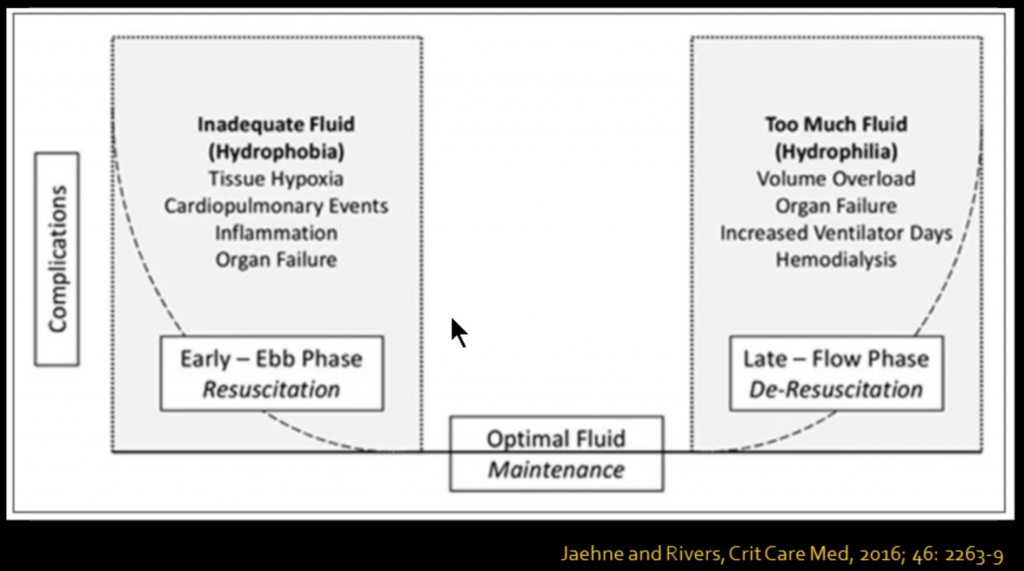
- Case Against Fluid Resuscitation (Except Early Resuscitation of Shock)
- First off, most of all animal models of sepsis are hypodynamic; whereas human sepsis is mostly hyperdynamic
- Starling curve is not perfect!
- ↑ cardiac filling P → ↑ natriuretic peptide→ breaks down of endothelial glycocalyx→ ↑ endothelial permeability
- Interstitial fluid→ pulmonary + tissue edema
- Tissue edema→ impaired oxygen and metabolite diffusion, tissue architecture distortion, impedance of capillary blood flow and lymphatic drainage, disturbed cell-cell interactions
- Kidney is affected: ↑ venous pressure→ ↑ renal subcapsular pressure→ ↓ RBF, ↓ GFR
- ↑ cardiac filling P → ↑ natriuretic peptide→ breaks down of endothelial glycocalyx→ ↑ endothelial permeability
- Major studies have failed to demonstrate support of massive IVF resus in sepsis:
- SOAP Study
- Multicenter cross-sectional cohort, 198 ICUs, 1,177 patients with sepsis
- Each 1L of positive fluid balance —> ↑10% odds of mortality
- VASST Study
- Retrospective review of a prospective randomized controlled trial (RCT)
- 778 patients with septic shock enrolled in vasopressin study
- Each ↑ quartile of fluid administration associated with ↑ mortality
- ICON study
- Prospective, cross-sectional cohort, 84 countries, 730 ICUs, 1,808 patients with sepsis (61% septic shock)
- Survivors had more negative fluid balance
- After the initial resuscitation, higher hazard ratio for death for each quartile of more fluid
- Prospective, cross-sectional cohort, 84 countries, 730 ICUs, 1,808 patients with sepsis (61% septic shock)
- Andrews, JAMA, 2017
- 212 patients in Zambia with sepsis
- RCT sepsis protocol (including aggressive fluids) vs usual care
- ↑ mortality in protocol group (48% vs 33%)
- Classic Trial
- Prospective RCT, 9 Scandinavian ICUs, 151 patients with septic shock
- Beyond initial resuscitation phase
- Standard care vs fluid boluses only if severe hypoperfusion
- Non-significant trend to lower mortality in fluid restriction, less AKI (significant)
- ProCESS, ARISE, ProMISe
- All 3 trials found that EGDT was equivocal to usual resuscitation
- FEAST trial
- 3600 children in Uganda, Kenya, or Tanzania (not in shock), RCT btw 20-40 cc/kg bolus vs. no bolus
- Fluid boluses significantly increased 48-hour mortality
- SOAP Study
- Question then becomes, should we fluid resus severe sepsis + septic shock?
- Of course we should!
- Early is best!!
- Leisman, Crit Care Med, 2017
- Observational cohort, 9 hospitals, 11,000 patients
- Early fluid resuscitation (< 120 mins) had lower mortality, less risk for mechanical ventilation, shorter hospital stay, less ICU days….
- Child, Clinicoecon Outcomes Res, 2017
- Volume OL = higher infection rate, increased morbidity, increased costs!
- Frutos-Vivar, Chest, 2006
- Prospective cohort, 37 hospitals, 8 countries
- 24 h fluid balance pre-extubation a risk factor of reintubation
- FACTT, NEJM, 2006
- Prospective, multicenter RCT of liberal vs conservative fluid management of ARDS
- 5 more ventilator-free days and 2.2 ICU-free days in liberal group
- Keeping CVP constant over several days actually represented a more positive fluid balance
- A declining CVP over several days actually represented an even fluid balance
- … this mostly applied to the NON-shock group
- No difference in need for dialysis to day 60, meaning more liberal fluids do NOT prevent renal failure
- Relative 10% increase in death at 60 days in the liberal fluid vs conservative fluid group (28.4% vs 25.5%)
- (though not statistically significant and not powered to detect a 10% relative difference in mortality)
- Prospective, multicenter RCT of liberal vs conservative fluid management of ARDS
- Of course we should!
- 54,130 expected deaths per year from ARDS, which would represent 5,413 excess deaths with liberal fluid
- There are only 3,443 drowning victims in the US annually
- More patients drown in the ICU than in the rest of the US!!
Suggested Reading
- National Heart, Lung, and Blood Institute Acute Respiratory Distress Syndrome (ARDS) Clinical Trials Network, Wiedemann HP, Wheeler AP, Bernard GR, Thompson BT, Hayden D, deBoisblanc B, Connors AF Jr, Hite RD, Harabin AL. Comparison of two fluid-management strategies in acute lung injury. N Engl J Med. 2006 Jun 15;354(24):2564-75. [Pubmed Link]
- Byrne L, Van Haren F. Fluid resuscitation in human sepsis: Time to rewrite history? Ann Intensive Care. 2017; 7: 4. [Pubmed Link]
- Chang DW, Huynh R, Sandoval E, Han N, Coil CJ, Spellberg BJ. Volume of fluids administered during resuscitation for severe sepsis and septic shock and the development of the acute respiratory distress syndrome. J Crit Care. 2014 Dec;29(6):1011-5. [Pubmed Link]