Today we have the distinct pleasure to welcome Neill Adhikari, MDCM, M.Sc., one of the world’s experts on critical care management in resource limited settings. Dr Adhikari is currently practicing as an intensivist at Sunnybrook Health Sciences Centre in the Interdepartmental Division of Critical Care at the University of Toronto. He also acts as an Associate scientist, Evaluative Clinical Sciences, Trauma, Emergency & Critical Care Research Program, at the Sunnybrook Research Institute where he focuses on critical care delivery in low-resource settings. Over his brief academic career Dr. Adhikari has been incredibly prolific in academic production, publishing over 180 peer-reviewed journal articles and accepting speaking engagements from around the globe. This afternoon we were fortunate to lure him down from Canada to speak on an exceedingly important topic: how can we address the devastation of sepsis in areas of the world where basic labs and clean water can often be a luxury and not a guarantee?
Podcast: Play in new window | Download
Subscribe: Apple Podcasts | RSS
Clinical Pearls (Assistance from Dr. Tony Basel)
- First issue notes that there is very little historical data on the incidence of sepsis in low income countries (LIC) and middle income countries (MIC), so it is difficult to truly understand the gravity of the problem.
- However, the amount of studies in LIC studies as grown exponentially over the last several years.
- Definition of Sepsis
- Consensus definition (updated in the last couple years)
- Suspected infection + Change in SOFA >2
- Issue: need Labs/interventions to get obtain SOFA scores
- Suspected infection + Change in SOFA >2
- WHO diagnosis (no labs, all clinically bsed)
- Suspected infection + 1 or more of:
- HR >100 bpm
- RR >24 Bpm
- Temp <36 or >38
- Suspected infection + 1 or more of:
- New developments for Sepsis 3
- Suspected infection + qSOFA >2
- AMS
- RR >20
- SBP <90
- Is QSOFA good or bad?
- Was created to prognosticate mortality, not for sepsis diagnosis
- Recent study in Gabon shows that
- Fever or hypothermia + 1 other SIRS + abx = mortality of 4.8%
- Sensitivity 87% + Specificity 75% (AUC 0.83)
- Minimally change to post-test probability
- Fever or hypothermia + 1 other SIRS + abx = mortality of 4.8%
- Suspected infection + qSOFA >2
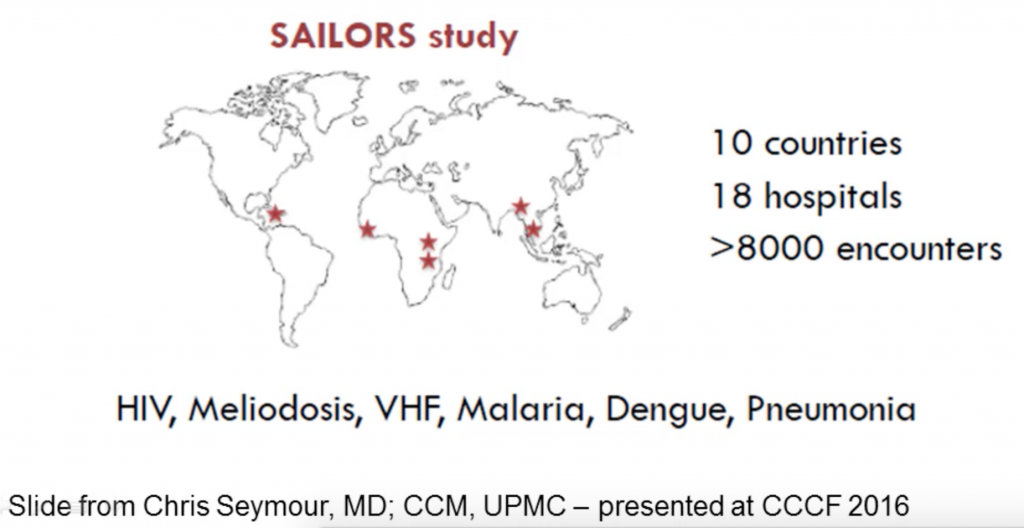
- The future is a study of qSOFA in low middle income countries with a wide variety of sepsis causing a:
- Consensus definition (updated in the last couple years)
- ARDS
- Berlin definition
- Requires CXR, ABG (P/F ratio), and access to echocardiography
- Not practical with minimal resources
- Kigali Modification of Berlin definition
- SpO2/FiO2 ratio (no ABG needed)
- Allows CXR or US
- More useful in resource limited countries (RLC)
- Requires CXR, ABG (P/F ratio), and access to echocardiography
- Berlin definition
- Epidemiology
- Sepsis is very underestimated in Global Data Base
- Example: A population of 850 million in Africa/Asia showed:
- 43 studies from 15 countries
- 36 ICUS in 31 cities
- Median admission rate: 461/yr
- Median ICU size: 8 beds
- Consensus data then shows that most sepsis does not occur in the ICUs of LICs or MICs, because it can’t (no ICU beds to hold them)
- Example: A population of 850 million in Africa/Asia showed:
- Unfortunately we do not have adequate population based data on Sepsis in resource limited countries
- From different sources we estimate that the LIC and MIC sepsis rate is about 13 million cases per year
- Measurement challenges
- Clinical databases don’t exist
- Hospital discharge databases don’t exist
- All we have is a death registry
- 5.3 million deaths per year GLOBALLY
- Difficult to stratify in LIC/MICs as “coding” and nomenclature is often complicated
- Data has shown that:
- Sepsis is very underestimated in Global Data Base
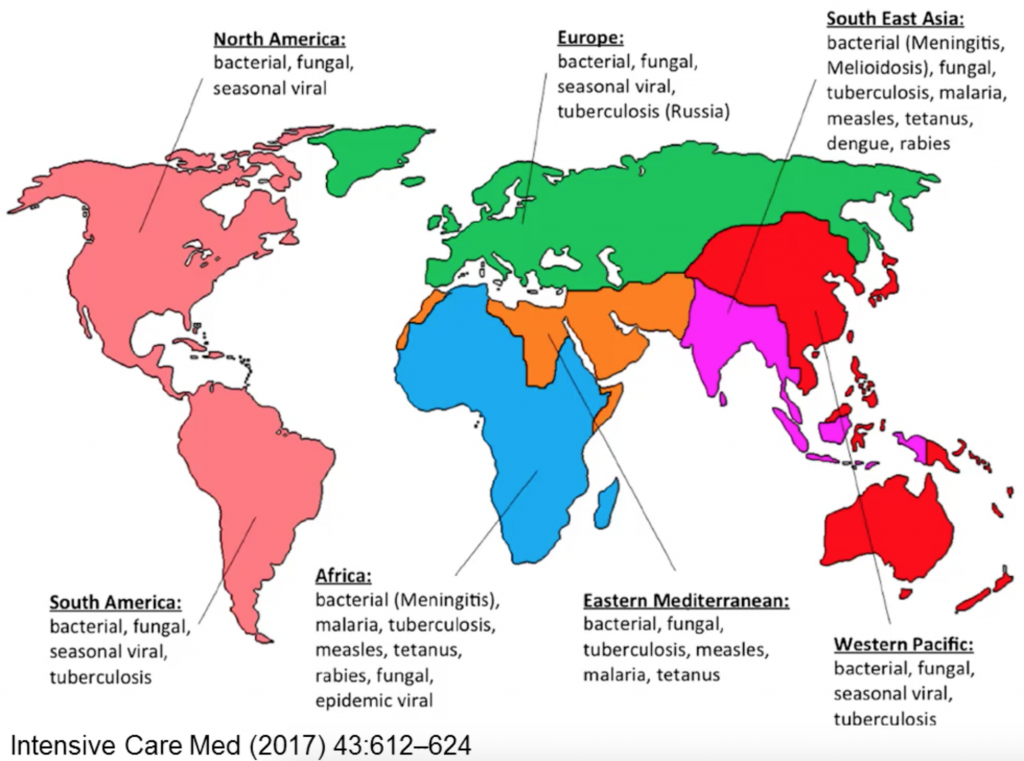
- Microbiology and Antimicrobial Resistance
-
- Bacteremia is difficult to diagnose in the LIC and MIC countries either due to lack of access to culturing materials or due to a simple lack of bacterial growth.
- The current antibiotic use is highest in higher income countries, but resistance is greatest in LIC! Why?
- Higher incidence of infection
- Higher prevalence of resistant bacteria
- High growth in antibiotic prescribing
- Lack of prescription controls
- Counterfeit drugs
- Poor infection prevention controls
- Laboratory capacities are limited and expensive (lack of vital antibiograms)
- Limit effect of the spread of disease with improvements to hospital cleaning protocols as well as cohort patients together with similar disease (ex: Cholera ward)
- The current antibiotic use is highest in higher income countries, but resistance is greatest in LIC! Why?
- Approaches to limit Antibiotic resistance in the ICU
- Infection control
- Hand Hygiene
- Active surveillance
- Contact precautions
- Cohorting
- Patient level
- Skin chlorhexidine
- Oral chlorhexidine
- SDD
- (No) ulcer Prophylaxis
- Proper antibiotic use
- Stewardship teams
- ‘Rotation’
- Better diagnostics
- Limit decision to start or duration of empiric therapy
- Microbiology labs
- Infection control
- Bacteremia is difficult to diagnose in the LIC and MIC countries either due to lack of access to culturing materials or due to a simple lack of bacterial growth.
- Treatment considerations in resource limited countries
- The current treatment guidelines available rely on data from High income countries and expert opinion, few are based on data from LICs
- One recent study from Haiti showed that standard sepsis goals (IVF, abx, etc) are rarely able to be met due to system limitations
- Very few studies in low income nations look at fluid resuscitation and antibiotic use, however nearly all show that:
- Fluid resuscitation is very sporadic, with some patients getting little fluid, while others getting a too much
- Antibiotic use differs wildly with up to >50 different antibiotic regimens
- Fixing the fluid problem with POC US with tele-medicine guidance, is this the future?
- The current treatment guidelines available rely on data from High income countries and expert opinion, few are based on data from LICs
Suggested Reading
- Dünser MW, Festic E, Dondorp A, Kissoon N, Ganbat T, Kwizera A, Haniffa R, Baker T, Schultz MJ; Global Intensive Care Working Group of European Society of Intensive Care Medicine. Recommendations for sepsis management in resource-limited settings. Intensive Care Med. 2012 Apr;38(4):557-74. [Pubmed Link]
- BJacob ST, Lim M, Banura P, Bhagwanjee S, Bion J, Cheng AC, Cohen H, Farrar J, Gove S, Hopewell P, Moore CC, Roth C, West TE. Integrating sepsis management recommendations into clinical care guidelines for district hospitals in resource-limited settings: the necessity to augment new guidelines with future research. BMC Med. 2013 Apr 18;11:107.
[Pubmed Link] - Murthy S, Adhikari NK. Global health care of the critically ill in low-resource settings. Ann Am Thorac Soc. 2013 Oct;10(5):509-13. [Pubmed Link]