Today with have the distinct pleasure to welcome a mentor of mine and a true expert in the field of critical care, Kevin K Chung, MD, FCCM, FACP, Colonel, Army. After finishing a fellowship in Critical Care Medicine at Walter Reed Army Medical Center, Dr. Chung was assigned to the US Army Institute of Surgical Research (USAISR) where he has served in the capacity of Medical Director of the Burn Intensive Care Unit, Task Area Manager of Clinical Trials in Burns and Trauma, and the Director of Research for the USAISR. He is currently the Chief of Medicine at Brooke Army Medical Center. COL Chung holds academic appointments at the Uniformed Services University of the Health Sciences as Professor of Medicine and Professor of Surgery. In his career, COL Chung has authored over 180 peer reviewed papers, authored 13 book chapters, and has been an invited speaker for over 85 lectures internationally.
We are exceedingly fortunate to have him in town to speak on ICU management of Burns. I am not exaggerating, Dr. Chung is the WORLD EXPERT on this topic. I recommend everyone, no matter your practice, take 60 minutes to appreciate the depth of knowledge passed along in this lecture. Burns don’t just present to burn centers!
Clinical Pearls (With help from Dr. Keegan Tupchong)
- Priorities of Burn Care
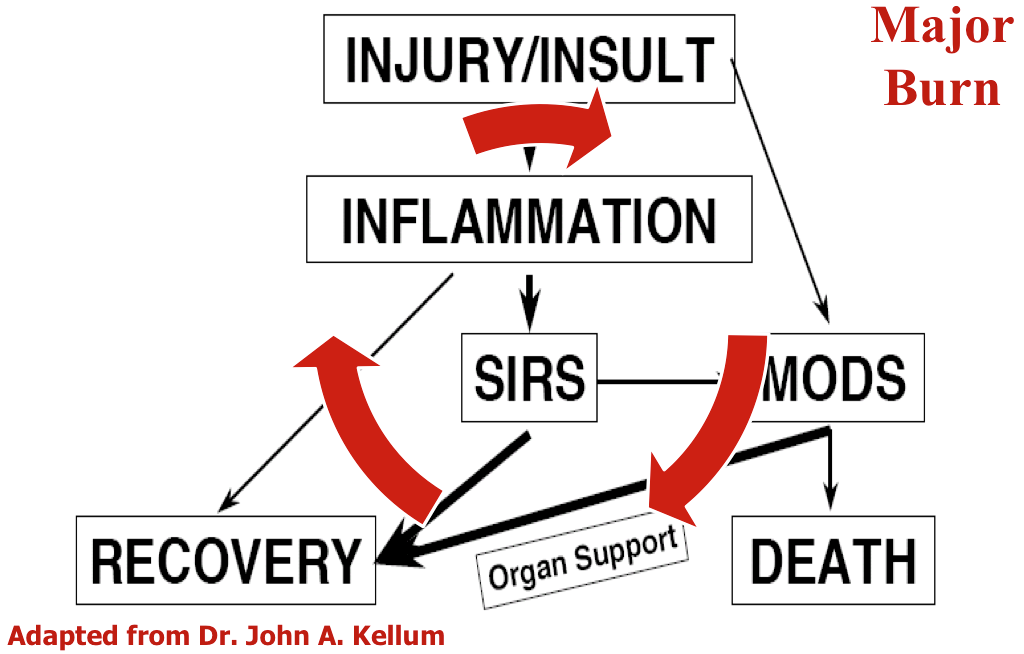
- Genomic response to burns is similar to trauma!
- If the burn wound is not addressed immediately then not much matters in terms of critical care interventions.
- Dead tissue must be removed and the wound bed must be covered!
- If this does not happen, the patient is at risk for multi-organ failure, electrolyte imbalance, and sepsis.
- Dead tissue must be removed and the wound bed must be covered!
- Host inflammatory response, including SIRS, continues until burn wounds are <10% open:
-
- The goal: close the burn wounds as soon as possible in a race against the overwhelming inflammation!
- Optimal resuscitation
- Capillary leak to BOTH burn tissue and non-burned tissues.
- Hypovolemic shock leads to extensive capillary leak and distributive shock.
- Parkland Formula:
- TBSA burned(%) x Wt (kg) x 2-4 mL
- Give 1/2 of total requirements in 1st 8 hours, then give 2nd half over next 16 hours.
- Does the starting rate matter? (2 ml or 4 ml?)
- Short answer, absolutely: Starting with a higher rate of fluid led to more total fluid given, and worse outcomes.
- Practically, not adhered to. However, still taught.
- TBSA burned(%) x Wt (kg) x 2-4 mL
- ISR Rule of 10
- Estimate burn size to nearest 10% (use rule of 9’s)
- Burn size x 10 = initial fluid rate (for adults 40-80 kg)
- For every 10 kg above 80 kg, add 100 cc/hr to rate.
- Hypotensive Hypovolemic Resus
- Goal is to maintain slight hypovolemia (lower thresholds).
- Tolerate the minimal MAP required to obtain organ perfusion.
- Avoid:
- Eschar Syndrome
- Extremity, thoracic, abdominal
- Urgent surgery, not emergent (1-2 hours)
- Compartment syndromes
- Orbital compartment syndrome (MASSIVE increased to IOP)
- Extremity compartment syndrome
- Abdominal compartment syndrome (ACS)
- > 45% TBSA +ACS = 100% mortality!
- Predictors of ACS:
- > 250 ml/kg in 24 hours (Ivy Index)
- > 6 cc/kg/%TBSA in 24 hours
- At 12 hours, project your 24 hour amount!
- Eschar Syndrome
- Goal is to maintain slight hypovolemia (lower thresholds).
- Control a “Runaway Resuscitation”
- Traditional Adjuncts: Albumin, FFP, Hypertonic Saline
- Novel Adjuncts:
- Vit C (decrease in overall fluid volumes)
- TPE/CVVH (first hemodilute the hemo-concentrated blood with IVF)
- Avoid fluid boluses (will extravasate)
- “Maintain organ perfusion using basic critical care principles… at the LEAST physiological cost”
- Capillary leak to BOTH burn tissue and non-burned tissues.
- Organ Support
- Acute kidney injury
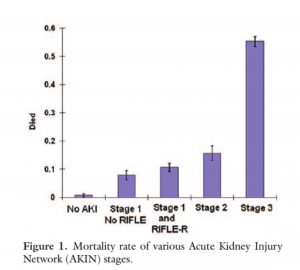
- AKIN in burns
- 1/3 of all burn patients will suffer AKI!
- Do small changes to creatinine matter?
- AKIN in burns
- Acute kidney injury
-
-
-
- Even a small increase to creatinine increases risk of mortality
- If HD is needed, mortality is 60%!
- Even a small increase to creatinine increases risk of mortality
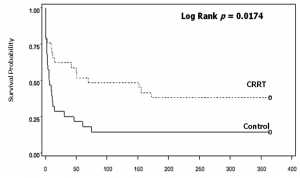
- CVVH in burns actually led to an increased survival when compared to SOC (no therapy):
-
-
-
-
-
- Even patients on multiple pressors would improve rapidly and be weaned off pressors with the use of CVVH.
- ARDS also improved significantly.
- New study: RCT of High Volume Hemofiltration (70 ml/kg/hr for 48 hours) vs. Standard CVVH (4k pts at 8 sites, 37 enrolled)
- Primary end point: vasopressor dependency index
- Index to inotropic score/MAP
- Rapidly improved vasopressor requirements!
- No change to circulating cytokines, proposed to improve metabolic requirements.
- Primary end point: vasopressor dependency index
- Other facts for CRRT use in burns (unpublished data):
- Not everyone goes on CRRT for AKI, some for volume OL.
- No matter who prescribes the CRRT (intensivist vs. nephrologist), the outcome is the same.
- 1/5 of patients will need RRT after discharge.
- 49% mortality for burn patients placed on CRRT (lower than expected).
-
- Inhalational injury
- Cilia decimated, mucus hypersecreted, mucosal destruction
- Preferred use of the VDR: high frequency percussive ventilator (HFPV)
- Inline, constant chest PT
- Recent study showed that HFPV vs ARDS low tidal volume ventilation
- “Conventional lung protective strategy insufficient in meeting ventilation or oxygenation goals”
- 29% of pts overall, or 64% of patients with inhalational injury.
- Strict adherence to Low Tidal Volume strategy extremely challenging in Burns!
- “Conventional lung protective strategy insufficient in meeting ventilation or oxygenation goals”
- 5 P’s of ARDS in Burns
- Lung Protection
- Paralyze
- Prune (dry out)
- Prone
- Put on ECMO
- MOST (Multiorgan support therapy)
- Single pass albumin dialysis (does not work well)
- Therapeutic plasma exchange (TPE)
- Molecular adsorbent recirculating system (M.A.R.S.)
- Nutrition
- Can’t just overfeed patients
- Need proper nutrition with exercise
- Can’t just overfeed patients
- Oxandrolone + Propranolol to mitigate the hyperadrenergic/hypercatabolic states
- Microbiology
- Resistant organisms
- Collectively known as “the end of modern medicine as we know it”
- Novel use through DARPA: Dialysis-Like Therapeutics
- Spleen on a chip
- Cytosorbents
- Aethlon Hemopurifier
- Fungal infections are common in the burn population
- Must have low suspicion
- Resistant organisms
-
Suggested Reading
- Rowan MP, Cancio LC, Elster EA, Burmeister DM, Rose LF, Natesan S, Chan RK, Christy RJ, Chung KK. Burn wound healing and treatment: review and advancements. Crit Care. 2015 Jun 12;19:243. [Pubmed Link]
- Chung KK, Lundy JB, Matson JR, Renz EM, White CE, King BT, Barillo DJ, Jones JA, Cancio LC, Blackbourne LH, Wolf SE. Continuous venovenous hemofiltration in severely burned patients with acute kidney injury: a cohort study. Crit Care. 2009;13(3):R62. [Pubmed Link]
- Walker PF, Buehner MF, Wood LA, Boyer NL, Driscoll IR, Lundy JB, Cancio LC, Chung KK. Diagnosis and management of inhalation injury: an updated review.Crit Care. 2015 Oct 28;19:351. [Pubmed Link]