Lewis Rubinson, MD, PhD, Professor of Medicine, Program in Trauma, R Adams Cowley Shock Trauma Center at the University of Maryland SOM and Vice President & Deputy Chief Clinical Officer at UMMC, presents the weekly multi-departmental critical care fellows’ lecture on “Status Asthmaticus.”
Lecture Summary by Dr. Jason Nam
SA Background and Basics
- Most ED visits (75%) for asthma do NOT require hospitalization. Inpatient mortality for asthma remains low (5%).
- This talk will focus on patients who require mechanical support. Life threatening status asthmaticus. Mostly younger patients.
- Historical predictors of life threatening asthma: HR >110, RR>25, PEF<50%, Pulsus Paradoxus >25. Not always best at predicting. Perhaps better predictor of risk is lack of peak flow improvement with albuterol.
- 3Ss of Asthma. Airflow obstruction due to swelling, bronchospasm, and Secretions.
- The immediate goals for
life threatening asthma:
- Improve airflow, reduce and avoid hyperinflation, and reduce inflammation.
- The pharm mainstays: SABA, systemic corticosteroids, inhaled short-acting anticholinergic, may consider IV Mg or terbutaline or heliox. Mechanical ventilation?
Non-invasive ventilation
- Benefit in COPD well-established.
- Potential benefits – improved mechanics without ETT, less HCAP.
- Potential pitfalls – gastric inflation and worse mechanics, aspiration, harder to limit RR and min ventilation.
- It requires proper patient selection and close monitoring.
- Consider if pH>=7.2. Close monitoring. Set iPAP to get Vt 6-8cc/kg. Set ePAP (PEEP) for trigger sensitivity. Watch RR and monitor pt very closely. Avoid in non-verbal patients.
- General recommendations to referring physicians: stop bagging patient esp at fast rate, NMBA paralysis, continuous SABA, VC-AC, set PIP alarm high, RR 8-12, Vt 6-7 cc/kg IBW.
How do patients with life-threatening SA die?
Hemodynamic collapse, barotrauma, progression of anoxic CNS injury; most do NOT have irreversible sequelae from hypercapnia.
Initiating invasive mechanical ventilation
- Induction with ketamine or propofol is reasonable
- May require intermittent NMBA.
- Do not manually ventilate at high rate peri-intubation.
- Anticipate high PIPs.
PIP vs Pplat in practice
High PIP w acceptable Pplat is generally not injurious; barotrauma tends to be correlated with elevated Pplat, not elev PIP with low Pplat.
Elevated PaCO2 usually does NOT kill. But hyperinflation does:
- Need sufficient expiratory time to allow lungs to empty to near FRC for next breath. Permissive hypercapnia.
- In truly life-threatening SA, lecturer uses Vol-AC, RR-10, Vt 6-7 cc/kg.
How to gauge when/how to modify settings
Air trapping due to mucus plugging and bronchospasm, dynamic hyperinflation,
Triggering with Auto-PEEP
- To initiate gas flow, the patient must generate an effort that exceeds the amount of auto-PEEP. So can increase PEEP to reduce work of trigger.
Is Extrinsic PEEP ok?
- PEEP can reduce work of trigger. PEEP could increase resistance to airflow during expiration.
- Permissive hypercapnia is not deliberate hypercapnia.
Other adjuncts?
- Heliox reduces turbulent flow. Unclear benefit.
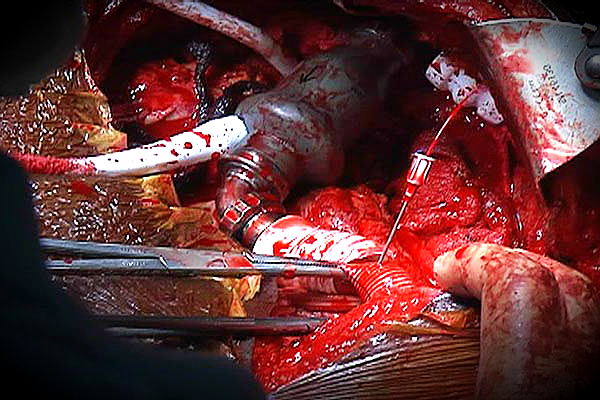
- Bronchoscopy- fatal cases of asthma can have tenacious mucus. Bronchoscopy can be considered.
- ECMO “Rescue”
References
- Brenner, Barry, Thomas Corbridge, and Antoine Kazzi. “Intubation and mechanical ventilation of the asthmatic patient in respiratory failure.” Proceedings of the American Thoracic Society 6.4 (2009): 371-379. https://www.ncbi.nlm.nih.gov/pubmed/19675347
- Leatherman, James. “Mechanical ventilation for severe asthma.” Chest 147.6 (2015): 1671-1680. https://www.ncbi.nlm.nih.gov/pubmed/26033128
Uploaded by Sami Safadi, MD
Podcast: Play in new window | Download
Subscribe: Apple Podcasts | RSS