Jonathan Chow, MD, Assistant Professor and Director, Critical Care Fellowship in the Division of Critical Care Medicine, Department of Anesthesiology at the University of Maryland SOM presents the weekly multi-departmental critical care fellows’ lecture on “When All Else Fails – Rescue Medications for Vasodilatory Shock.”
Lecture Summary by Dr. Jason Nam
Types of shock
- Obstructive Shock (2%)
- Hypovolemic Shock (16%)
- Cardiogenic Shock (16%)
- Distributive Shock (66%)
- Septic (62%) – most common shock in the ICU
- Non-septic (4%)
Why is shock so deadly?
- Low BP increases likelihood of AKI and myocardial injury.
- Increased mortality and
norepinephrine-refractory vasoplegic syndrome.
- Prolonged post-op vasoplegic syndrome leads to multiorgan failure and increased mortality. Vasoplegic syndrome after off-pump coronary artery bypass surgery: a rising threat.
- Other complications
- Ischemic skin lesions developing in 30% of ICU patients with catecholamine-resistant vasodilatory shock.
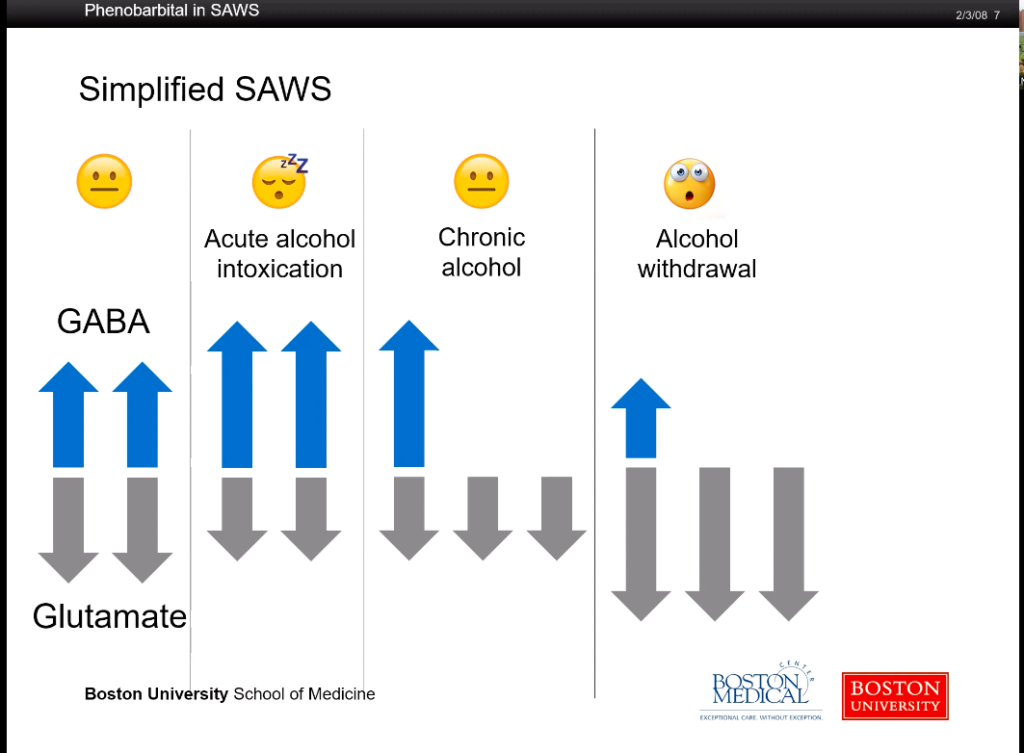
Catecholamine Resistance
- Other adjuncts (see below)
- Novel vasopressors such as angiotensin II When All Else Fails: Novel Use of Angiotensin II for Vasodilatory Shock: A Case Report.
Rescue Medications for Vasodilatory Shock
- Methylene Blue:
- Methylene blue decreased nitric oxide by inhibiting nitric oxide-stimulated soluble guanylyl cyclase.
- May reduce mortality after cardiac surgery. Methylene blue reduces mortality and morbidity in vasoplegic patients after cardiac surgery.
- May reduce ICU length of stay. Preoperative methylene blue administration in patients at high risk for vasoplegic syndrome during cardiac surgery.
- No real Level 1 evidence on MB. Use of methylene blue in sepsis: a systematic review.
- Vitamin B12
- Thought to be due to NO scavenging. Use of Hydroxocobalamin (Vitamin B12a) in Patients With Vasopressor Refractory Hypotension After Cardiopulmonary Bypass: A Case Series.
- Thiamine and Vitamin C
- Combination of vitamin C and thiamine is being used to treat septic shock Hydrocortisone, Vitamin C, and Thiamine for the Treatment of Severe Sepsis and Septic Shock: A Retrospective Before-After Study.
- Vitamin C is a potent antioxidant and free radical scavenger. It also increases sensitivity to glucocorticoids.
- Thiamine deficiency also common in sepsis.
- The above retrospective study showed that: NE requirements decreased, SOFA scores improved, and over 30% reduction in mortality.
- VICTAS: an enrolling clinical trial to study the above
Angiotensin II
- Angiotensin II decreases NE requirements. Kidney releases renin in low perfusion states. Occurs in pulmonary and renal endothelium. Angiotensin II causes ADH secretion and increases MAP.
- ATHOS is a study on angiotensin II use. Intravenous angiotensin II for the treatment of high-output shock (ATHOS trial): a pilot study.. Angiotensin II for the Treatment of Vasodilatory Shock. Sickest and most septic patients in ICU. Treatment arm received Angiotensin II plus standard of care vasopressors. 70% reached MAP target by hour 3. Median time was 5 minutes. Fast onset and offset. Saw improvement in SOFA score. Decreased background vasopressors. Not powered to detect for any mortality.
- Ang II has cost comparable to vasopressin and used for about 2 days. $1500 daily. Vasopressin costs $750 daily. Timing- should be started earlier in hospital course.
References
- Marik, Paul E., et al. “Hydrocortisone, vitamin C, and thiamine for the treatment of severe sepsis and septic shock: a retrospective before-after study.” Chest 151.6 (2017): 1229-1238.
https://www.ncbi.nlm.nih.gov/pubmed/27940189 - Khanna, Ashish, et al. “Angiotensin II for the treatment of vasodilatory shock.” New England Journal of Medicine 377.5 (2017): 419-430.
https://www.ncbi.nlm.nih.gov/pubmed/28528561 - Hosseinian, Leila, et al. “Methylene blue: magic bullet for vasoplegia?.” Anesthesia & Analgesia122.1 (2016): 194-201.
https://www.ncbi.nlm.nih.gov/pubmed/26678471
Uploaded by Sami Safadi, MD
Podcast: Play in new window | Download
Subscribe: Apple Podcasts | RSS