Seth J Koenig, MD, Professor, Dept of Medicine and Cardiovascular and Thoracic Surgery; Professor of Medicine, Donald and Barbara Zucker SOM at Hofstra/Northwell; Director, Acute Lung Injury Center, Northwell Health; and Director, MICU at the Long Island Jewish Medical Center, presents on “Transesophageal Echocardiography in the Intensive Care Unit”.
Lecture Summary: TEE in the ICU – Seth Koenig
Summary by Dr. Keegan Tupchong
TEE in the ICU
- not dangerous
- not hard
- can be mastered by non-cardiologists
- data show that it helps clinical decision-making
Reasons to learn TEE
- Anyone who is critically ill probably deserves POCUS
- TEE is used for all ECMO cannulations at Long Island Jewish Medical Center
- You will be left behind if you
don’t start learning TEE in fellowship
- the same paradigm used to exist for learning general POCUS as well as critical care TTE, and now everyone has POCUS in their ICUs
- Taking good care of a patient
means that at least you must know what is wrong
- while it does not replace clinical skills, TEE as an adjunct can give you the data needed to become a better clinician
- TEE is much less dangerous and
complicated than many other procedures required by ABIM:
- airway management
- CVCs, A-lines, PACs
- ventilator management
- There may not be an RCT showing
improved outcomes with TEE but …
- this has yet to be shown for ventilators, CT scans
- “we hold these truths to be self-evident” and assume that they benefit patients
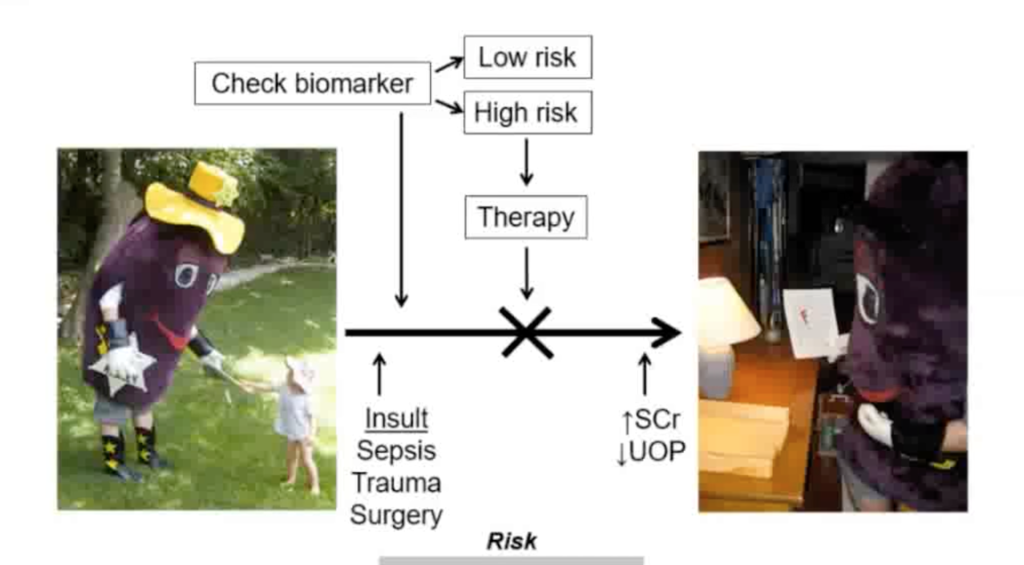
- Categorizing the shock state is
essential
- “if you understand the shock state then you know how to treat the shock state”
- diagnosis of life-threatening diseases saves lives
- hemodynamic profiles change constantly
TEE image acquisition:
- There are different types of gross movements
- vertical (advance/withdraw the probe)
- rotational (turning the probe/beam plane)
- anteroflexion/retroflexion
- lateral flexion
- multi beam
- Beam path is the opposite of TTE (from inside the chest pointed outwards)
Ten Reasons for Performing Hemodynamic Monitoring Using TEE (Vignon, et al, ICM, 2017)
- TEE provides a unique window to the heart and great vessels (e.g. dissection)
- TEE provides unparalleled information on the mechanism of circulatory failure (e.g. saddle PE, too unstable to go to CT)
- TEE allows reproducible and sequential hemodynamic assessments
- (e.g. slightly large RV but normal SV (normal HR, VTI) may point towards vasodilatory rather than obstructive shock (with old RV dysfunction))
- TEE predicts fluid responsiveness (better than any other cardiac output monitoring paradigm)
- TEE is best suited to quantitatively assess cardiac function (e.g. degree of severity of mitral regurgitation)
- TEE is key to identifying RV dysfunction at the origin of low flow states (e.g. large ASD)
- TEE is the only possibility to monitor hemodynamic status in the context of the use of ECMO (e.g. cannula placement)
- TEE is quicker and easier to initiate than other monitoring modalities, and less operator dependent than TTE
- Miniaturized TEE probes allow prolonged hemodynamic monitoring
- TEE potentially improves ICU performance
Complications
- Risk of death = 0.0098% (cardiology TEE)
- Several large studies combined show ~1 death in 30,000 patients
- All complications of any type =
2.8% (lower than for central lines, transbronchial biopsies, etc…)
- hypoxemia
- hypo/hypertension
- dislodged NGT
- minor upper airway injury
Diagnostic Accuracy of and Therapeutic Impact of TTE and TEE in Mechanically Ventilated Patients in the ICU (Vignon, et al, ICM, 2017)
- no deaths from TEE
- when TTE could not solve a clinical problem, TEE was performed, and the majority were solved with TEE
- Only 4 views are likely needed
- mid-esophageal 4 chamber (RV and LV size and function, mitral valve)
- mid-esophageal long axis (aortic valve)
- bicaval (preload responsiveness)
- transgastric short axis (RV and LV size and function)
Impact of Critical Care TEE in Medical-Surgical ICU Patients: Characteristics and Results from 274 Consecutive Examinations (Arntfield, et al, J ICM, 2018 )
- TEE aids clinicians in decision-making (e.g. dissection)
- Focused TEE by Emergency Physicians is Feasible and Clinically Influential
- Takes 30-35 TEE studies to achieve competence for non-cardiologists
Critical Care Fellow Training and Utilization at Long Island Jewish:
- 3 modules, ~4 TEE views in each
- each performs 10 exams on a simulator
- most can master the TEE exam in real patients after 10-20 exams (as opposed to 30-35, above)
Feasibility, Safety, and Utility of Critical Care TEE Performed by Pulmonary and Critical Care Fellows in the ICU (Garcia, et al, Chest, 2017)
- 129 exams at LIJ by fellows
- 100% success in insertion and image acquisition
- TEE led to a change in clinical management
- 35% therapeutic change, 65% therapeutic no change (a negative exam still gives you lots of information)
References
Mayo, Paul H., Mangala Narasimhan, and Seth Koenig. “Critical care transesophageal echocardiography.” Chest 148.5 (2015): 1323-1332. https://www.sciencedirect.com/science/article/pii/S0012369215502444
Jaidka, Atul, et al. “Better with Ultrasound: Transesophageal Echocardiography.” Chest (2018). https://www.sciencedirect.com/science/article/pii/S0012369218325637
Garcia, Yunuen Aguilera, et al. “Feasibility, safety, and utility of advanced critical care transesophageal echocardiography performed by pulmonary/critical care fellows in a medical ICU.” Chest 152.4 (2017): 736-741. https://www.sciencedirect.com/science/article/pii/S0012369217312059
Uploaded by Sami Safadi, MD
Podcast: Play in new window | Download
Subscribe: Apple Podcasts | RSS