[tab_nav type=”6-up”][tab_nav_item title=”Clinical Case” active=”true”][tab_nav_item title=”Case 1 Answer” active=””][tab_nav_item title=”Case 2″ active=””][tab_nav_item title=”Case 2 Answer” active=””][tab_nav_item title=”Case 3″ active=””][tab_nav_item title=”Case 3 Answer” active=””][/tab_nav][tabs][tab active=”true”]As we continue through our trek into ECMOvember you are all slowly becoming experts in extracorporally oxygenating people! This post will introduce three common ECMO disasters that are easy to treat…. if they are caught early….
Your newest patient is a 32 year male who arrested while riding the tram next to the hospital. Luckily two doctors who were headed home after a long shift started CPR immediately (true story). The tram operator was able to get EMS on scene immediately as an ambulance was just leaving the hospital and the patient was taken the short distance to the ED where an ICU team met him and placed him on VA-ECMO under eCPR protocol (extracorporeal cardiopulmonary resuscitation). You meet the patient in the ICU and see that he has a 15 F catheter into the right femoral artery as well as a multistage catheter placed into the right femoral vein.
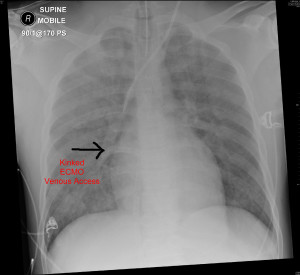
You are called to the viewing station to check a CXR to see if his endotracheal tube is in place and see:
Problem #1: The ETT is in good position, but something else catches your eye…. can you spot it?
[/tab][tab]
Answer
When placed in the femoral vein for venous return of VA-ECMO, the multistage catheter tip should be placed near the junction of the inferior vena cava and right atrium. In this patient the cannula was placed so deep that it was actually kinking in the right atrium! This will not only lead to poor flows but also risk damaging the myocardium and causing arrhythmias.
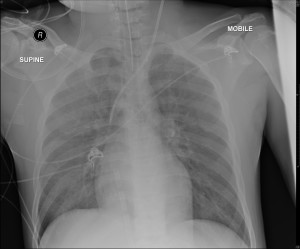
With early identification and re-positioning the cannula can now be seen in near perfect placement:
[/tab][tab]
After dodging the first catastrophe you go for a cup of coffee knowing it could be a LONG night. Just as you are about to take the first sip the nurse grabs you and tells you something is wrong!
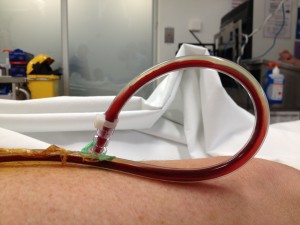
Problem #2: You are greeted at the door with the following site on the Rotaflow pump:
You run into the room, look down at the cannulas and see:
What is going on here? What can you do? [/tab]
[tab]
Signs of Access Insufficiency: 1) Flow fluctuations on the pump (inability to hold a consistent flow rate) 2) Kicking of the venous access cannula (as seen above), and 3) hemolysis (as measured by increased free Hgb).
This is imperative to recognize early as treatment needs to be implemented immediately.
The most common causes can be broken down to
- Vascular: dehydration, excessive bleeding, excessive vasodilation
- Mechanical: kinked cannula (common after a turn), cannula size too small, RPM turned too high
- Pressure: ↑ cardiac pressures (tamponade), ↑ abdominal pressures (IAH), ↑ thoracic pressure (coughing)
- VA ECMO only problems: Severe aortic regurgitation or severe pulmonary hemorrhage
The final caveat is to not mistake kicking for transmitted pulsations from the recovering heart, as seen below:
This is a normal occurrence and may intensify as the heart function recovers!
[/tab]
[tab]
Problem #3: You are extremely satisfied having figured that out and are about to leave the room when you take one last peak at the patient and see:
Ignoring the nail polish, what do you see?
You think you have the diagnosis figured out when you pull back the blankets to look at the access sites and see:
What does this show and does it confirm what you suspected? What is your next immediate action?!? [/tab][tab]
There is obvious color differential btw the feet indicative of arterial compromise! The left foot is significantly more pale:
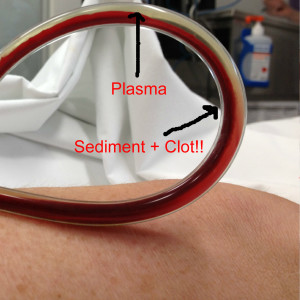
This is most likely due to the fact that the back flow cannula is completely clotted off as shown below:
The differential is limited and vascular surgery consult with STAT arterial doppler imaging is required to evaluate for arterial embolization downstream from the clot.
The only treatment is immediate revascularization. This is best done immediately, and can often be achieved by clamping the circuit and replacing the back flow cannula under sterile technique. Depending on the length of the ischemia, you may need to monitor for compartment syndrome with serial myoglobin, CK, and measurements renal function. [/tab][/tabs]
Thanks to The Alfred faculty and staff for their support, especially Vin Pellegrino, Steve Bernard, and Jayne Sheldrake. Thanks also goes out to Chris Nickson over at LITFL for the tips and tricks!