Traditionally, the approach to pulseless electrical activity (PEA) has been to focus on reversible causes of arrest — the “Hs and Ts”.
This makes sense in theory, but, in practice, remembering a list of 10 things during a hectic code probably isn’t the most productive approach to correct the underlying etiology. Also, many of the “Hs and Ts” are likely consequences and not causes of arrest, and others don’t readily apply to the inpatient population (I hope your patients don’t inadvertently become severely hypothermic!).
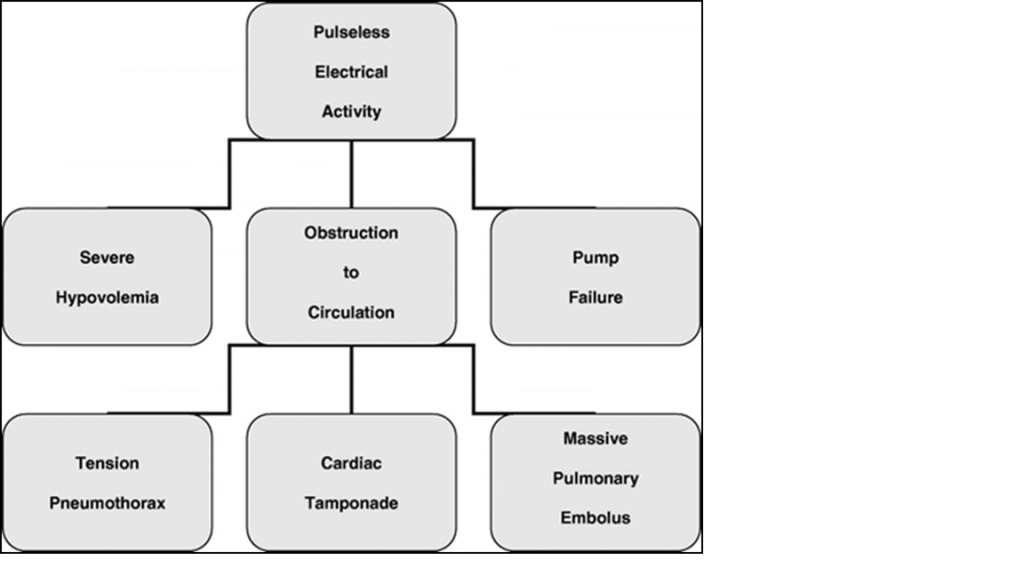
Another way to remember the reversible causes is the “3 and 3 rule”. The same logic as applied to renal failure works very well here; consider pre-cardiac, cardiac, and post-cardiac causes of PEA:
- “Pre-cardiac” is hypovolemia
- “Cardiac” is pump failure due to:
- muscle (e.g., massive MI, acidosis)
- valves
- dysrhythmia
- “Post-cardiac” also nicely breaks down into three causes:
- tension pneumothorax
- cardiac tamponade
- massive pulmonary embolism
http://resus.me/the-real-shocked-patient/
How do you differentiate among these causes?
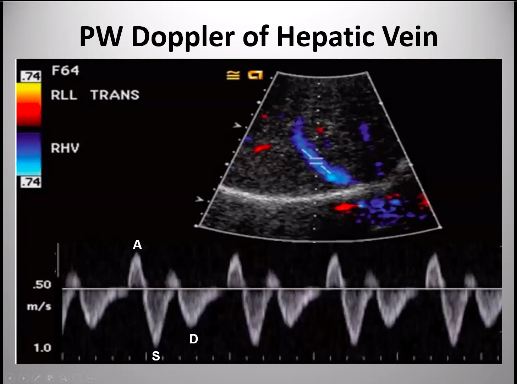
Bedside ultrasound! In addition to your targeted physical exam during a pulse check, should readily differentiate all the causes:
- If the myocardium isn’t moving, you know that primary pump failure is most likely.
- The other treatable causes of PEA likely won’t be subtle, with a large pericardial effusion for tamponade (with the caveat that true tamponade should have right atrial collapse) or distended right ventricle for massive pulmonary emboli.
In short, the “3 and 3 rule” is a quicker, easier way to remember the causes of treatable PEA arrest that can be quickly applied at the bedside.
References
- Neumar RW, Otto CW, Link MS, Kronick SL, Shuster M, Callaway CW, Kudenchuk PJ, Ornato JP, McNally B, Silvers SM, Passman RS, White RD, Hess EP, Tang W, Davis D, Sinz E, Morrison LJ. Part 8: adult advanced cardiovascular life support: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 2010;122(18 Suppl 3):S729-67
- Desbiens NA. Simplifying the diagnosis and management of pulseless electrical activity in adults: a qualitative review. Critical Care Medicine 2008;36(2):391-6