[tab_nav type=”two-up”][tab_nav_item title=”Clinical Case” active=”true”][tab_nav_item title=”Answer” active=””][/tab_nav][tabs][tab active=”true”]
You are working in the MICU on a relatively quiet Sunday night, turn the lights off and just as you are about to close your eyes the pager lights up: “septic pt in the ED- please come evaluate for admission”….
You wipe your eyes and venture down to room 23 and see an elderly female in a state of obtundation. The ED team is preparing to intubate and hand you the chart with the following synopsis:
“72 yo F, Vietnamese speaking, unknown PMHx, found by her landlord to be nearly unresponsive and EMS was called. On arrival pt was severely hypothermic (34 C), bradycardic (45), hypertensive (174/103), hypoglycemic, altered mental status, and decreased respiratory rate (8). Pt was given D50 and bought to the ED”
You do a quick exam of the labs and see hyponatremia, hypercapnea, elevated creatinine, elevated creatinine phosphokinase, continued hypoglycemia, and finally signs of a UTI. On a quick exam she has clear lungs, a slow heart, signs of significant peripheral edema, and a very tender abdomen. The only unusual finding is her eyes:

You are otherwise unimpressed: “sepsis from a urinary source, recommend CT abdomen, fluids, antibiotics, and admission to ICU”. You then enter the elevator to make your trek back to the ICU. Somewhere around floor 4 the REAL diagnosis hits you int he face! You rush out of the elevator and scramble down the stairs back to the ED!!
What is really going on here? What labs are you missing? What must be started ASAP or this patient might not make it to the next morning?……….
[/tab]
[tab]
Myxedema Coma
- Hypothyroidism: general slowing of metabolic functions → mental and physical depression
- Myxedema coma: severely decompensated hypothyroidism with hemodynamic instability coupled with the inability to maintain homeostasis
- Mortality: 60-70% with delayed diagnosis, improved to 20-25% with early recognition
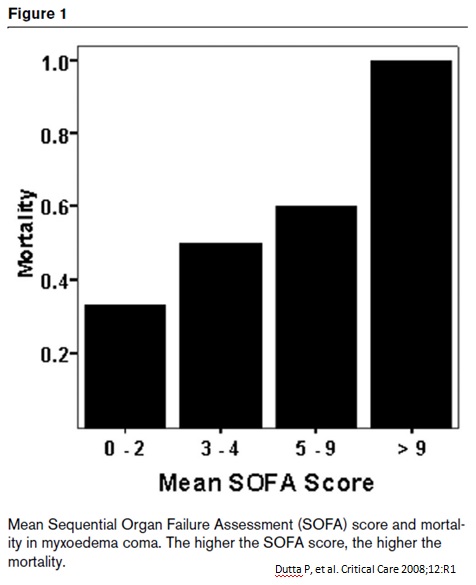
- Dutta and colleagues determined that the following risk factors yield a higher rate of mortality
- advanced age
- hemodynamic instability
- severe bradycardia
- respiratory dysfunction requiring intubation
- hypothermia
- sepsis
- depressed GCS
- higher APACHE II scores
- Dutta and colleagues determined that the following risk factors yield a higher rate of mortality
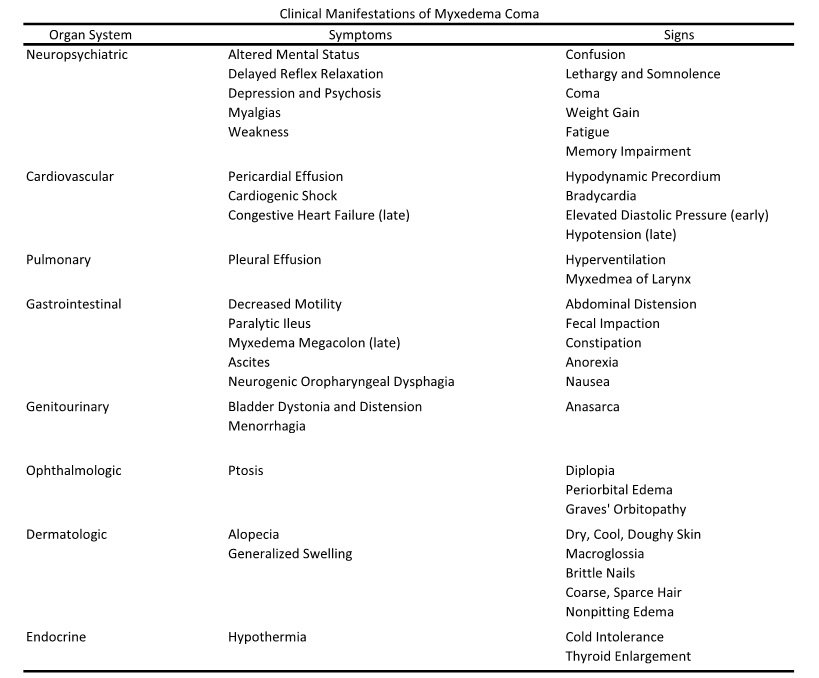
- Presentation:
- Overall depression to global physiological function:
- Hypothermia, bradycardia, hypertension, respiratory acidosis, and AMS
- Classic hypothyroidism features: dry skin, brittle nails, hair loss, delayed deep tendon reflexes, goiter
- Mucin deposits → nondependent sites of non-pitting edema (myxedema)
- Global physiological failure:
- Decreased CNS sensitivity to hypoxia and hypercarbia + macroglossia + respiratory muscle weakness → respiratory failure
- Vascular permeability → effusions and ascites
- Renal injury → water retention and hyponatremia
- Depressed ionotropic and chronotropic myocardium → cardiogenic collapse
- Gastrointestinal dysmotility → paralytic ileus
- Can mimic a surgical abdomen and result in unnecessary surgery
- Overall depression to global physiological function:
** HINT: Graves’ orbitopathy (like on our patient) does NOT resolve with treatment of Grave’s disease- can be indicative of current thyroid depressant treatments **
- Laboratory diagnosis:
- Severely depressed levels of both T4 and T3, with an elevation to TSH
- However, lab values do not correlate with level of disease
- Hyponatremia and elevations to creatinine (renal dysfunction)
- Normocytic anemia
- Alteration to von Willebrand’s factor synthesis (due to low thyroxine levels) → coagulopathies
- Decreased gluconeogenesis → hypoglycemia
- Severely depressed levels of both T4 and T3, with an elevation to TSH
- Causes:
- Infection is most common inciting event: PNA, cellulitis, UTI
- Systemic insults: cerebrovascular accidents, congestive heart failure, gastrointestinal bleeds
- Medications: sedative-hypnotics, lithium, abrupt discontinuation of thyroid supplements
- Hypothermia during the winter months is also thought to be responsible for a large number of cases
- Due to an age-related loss of temperature regulation + depressed heat production of hypothroidism
- Bok Choy (recent NEJM article!): contains cyanates, nitriles, and oxazolidines which inhibit iodine uptake in the thyroid
- Treatment:
- Prompt admission to a critical care setting + aggressive hemodynamic support!
- MUST start treatments BEFORE laboratory confirmation
- Classic 3-tiered treatment plan:
- Early initiation of thyroid replacement
- Symptomatic support of organ dysfunction
- Management of the inciting event
- Thyroid replacement general principles:
- Liothyronine (LT3)
- Immediate bioavailability = faster effect
- Easily crosses blood brain barrier
- Increased CV complications: arrhythmia and ischemia (increased risk with vasopressor use)
- Levothyroxine (LT4)
- Less CV complications
- Requires 5’-deiodination to active state (T3)
- Not easily transported across the blood brain barrier → prolonged CNS symptoms
- Parenteral > Oral administration preferred due to unpredictable GI absorption
- Plan: Start with parenteral of LT3 and LT4 (combo) with early switch to PO LT4
- Increased CV complications with parenteral form of either replacement!
** TAKE HOME: Hyponatremia + Hypothermia + AMS ± Hypercapnea = Myxedema Coma on differential **
- Liothyronine (LT3)
References
- Dutta P, Bhansali A, Masoodi SR, Bhadada S, Sharma N, Rajput R. Predictors of outcome in myxedema coma: a study from a tertiary care center. Critical Care 2008;12:R1.
- Kwaku MP, Burman KD. Myxedema coma. Journal of Intensive Care Medicine 2007;22:224-231.
- Wartofsky L. Myxedema coma. Endocrinology Metabolism Clinics of North America 2006;35:687-698.
[/tab][/tabs]