[x_text]Today we are fortunate to have Dr. Steven M. Frank, an associate professor of anesthesiology and critical care medicine at the Johns Hopkins University School of Medicine. Acting under the role of director of 3 vital programs: Bloodless Medicine and Surgery Program, Interdisciplinary Blood Management Program, and of Perioperative Blood Management Services, Dr Frank has saved resources, time, money, and (as you will see) countless lives by limiting blood transfusions throughout the immense Hopkins empire of hospitals. Dr. Frank will harness the knowledge gained from over a 100 personal publications on blood use and blood product management to give you one of the most informative 50 minutes of 2015. [/x_text]
[x_text][/x_text][x_text]
Podcast: Play in new window | Download
Subscribe: Apple Podcasts | RSS
[/x_text][x_text class=”left-text “]
Clinical Pearls
Clinical Pearls
- The Joint Commision notes that blood product administration is the #1 most overused practice in all of medicine (over even abx for URIs!!)
- Blood production management is the ONLY intervention in medicine that achieves: Reduced Risk, Improved Outcomes, and Cost Savings!
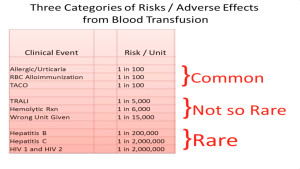
- Relative Risk of serious reactions: Hep C/HIV are minuscule (same as death by lightning strike) in comparison to the top 2 killers: 1) TRALI (10% fatal) and 2) TACO!
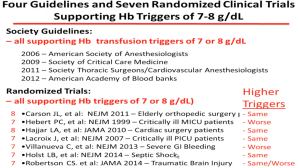
- All societies agree with a Hgb trigger of 7 (8 with CV dz) for RBC transfusion
- SEVEN major publications show equal or better outcomes compared to higher triggers!
- Storage lesions are significant!
- RBC lose deformability and are more rigid, often stuck at 7μm (where capillaries are 5-10μm) and is NOT reversible
- ⇓ 2,3 DPG: 90% depletion in stored blood, leads to a left shift of Hgb/O2 curve (more affinity to hold onto O2
- This decrease is evident even 3 days s/p transfusion
- ⇓ NO-Hgb: this makes Hgb a NO scavenger and leads to vasoconstrictio
- ⇑ endothelial adherence of RBC
- ⇑ aggregatability (pro-thrombotic)
- Massive transfusion: 50% mortality after 50 units!
- Every 10 units ~ 10% increase in mortality!
- Some ideas to reduce reliance on RBC transfusion:
- Tx anemia with Fe pills pre-elective surgery ($5 tx vs $500 for RBCs)
- Less invasive surgery as first option
- Blood salvage devices
- ⇓ Phlebotomy draws
- The avg ICU pt loses 1% of blood volume per day (the same as is generated by erythropoiesis!)
- Most blood loss is waste pre-lab draws!
- CPOE creation with clinical decision support
- Antifibrinolytics (TXA or Amicar when indicated!)
- POC testing (TEG)
- Audits with feedback (and public shaming of outliers)
- Education!
[/x_text]
[x_text]Suggested Reading
- Carson JL, Terrin ML, Noveck H, Sanders DW, Chaitman BR, Rhoads GG, Nemo G, Dragert K, Beaupre L, Hildebrand K, Macaulay W, Lewis C, Cook DR, Dobbin G, Zakriya KJ, Apple FS, Horney RA, Magaziner J; FOCUS Investigators. Liberal or Restrictive Transfusion in High-Risk Patients after Hip Surgery. N Engl J Med. 2011 Dec 29;365(26):2453-62. [NEJM Link]
- Frank SM, Savage WJ, Rothschild JA, Rivers RJ, Ness PM, Paul SL, Ulatowski JA. Variability in blood and blood component utilization as assessed by an anesthesia information management system. Anesthesiology. 2012 Jul;117(1):99-106. [PubMed Link]
- Hébert PC1, Wells G, Blajchman MA, Marshall J, Martin C, Pagliarello G, Tweeddale M, Schweitzer I, Yetisir E. A multicenter, randomized, controlled clinical trial of transfusion requirements in critical care. Transfusion Requirements in Critical Care Investigators, Canadian Critical Care Trials Group. N Engl J Med. 1999 Feb 11;340(6):409-17. [NEJM Link]
[/x_text]



