Today we were able to convince Dr. Gunjan Parikh to grace the lecture hall and give us an amazing update in the field of neurocritical care! Dr. Parikh is an Assistant Professor of Neurology at the University of Maryland Medical Center where he primarily works in the Neurocritical ICU and Neurotrauma ICU. Today we will go through everything from the newest studies of tPA use in intracranial hemorrhage to the use of diabetic medications to improve outcomes in CVA patients. This talk cannot be missed no matter which ICU you find yourself in!
Clinical Pearls (assisted by Dr. Helen Prevas)
Post arrest
- Brain injury post-arrest:
- Caused by hypoperfusion & energy failure
- Effects areas with high metabolism (basal ganglia, etc.)
- Targeted Temp Management (TTM)
- 36C is ideal x 24 hours (then 48-72 hrs normothermia)
- Caveat: must delay neuroprognostication
- Caused by hypoperfusion & energy failure
- Prognostication (multimodal):
- EEG is useful in 1st 12h, during rewarming, @ 72h and beyond
- SSEPs is done @ 72hrs when pt lacks eye opening
- Assesses integrity of reticular activating system by stimulating median nerve & following somatosensory pathway
- Biomarkers
- Trend important ones (NSE, S100 beta) – note not very specific
- Imaging
- MRI @ day 3 (more commonly @ 5-6)
- Use tensor imaging to look at white matter pathways
- MRI @ day 3 (more commonly @ 5-6)
TBI
- Changing demographic to the older, less severe pts
- Basics:
- Monro-Kellie hypothesis: fixed cranial volume, so increase in either blood, CSF, or brain parenchymal volume must decrease others or result in elevated ICP)
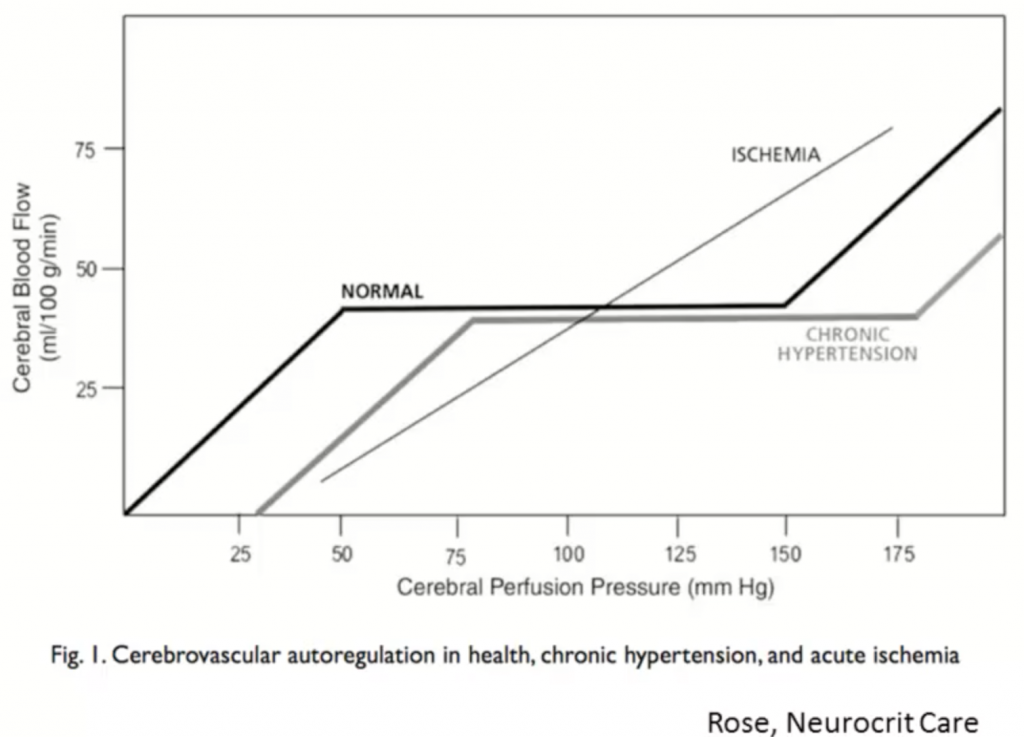
- Auto regulation of cerebral perfusion
- Goal to prevent secondary injury
- Elevated ICP management (low levels of evidence)
- Hypothermia→ will decrease ICP ~10 mmHg
- NABISH II – very early hypothermia, potential harm so trial ended early
- EuroTherm – hypothermia before osmotherapy vs osmotherapy alone (many osmo pts crossed over)
- Failed as a therapy
- Therefore: Used only when pt is refractory (3rd tier treatment)
- Difficult to phenotype, attempting to create a registry
ICH
- Hemorrhagic CVA
- 10-15% all strokes; 40% 30 day mortality; ~20% independent at 6 mos
- Outcome mainly affected by ICH volume and Intraventricular hemorrhage
- ICH score (at baseline)
- GCS
- ICH volume (≥ or < 30)
- IVH
- Location (infratentorial?)
- Age (≥ or < 80)
- Clear III (unpublished)
- Clot removal → EVD and tPA
- Decreased mortality but no change in disability (modified Rankin 4-5)
- MISTIE III trial (Phase 3 now enrolling)
- Goal: reduce ICH volume (has been shown to decrease disability)
- Again: Clot removal with EVD and prolonged tPA use
- ICH score (at baseline)
- BP management: ICH = loss of autoregulation
- Interact II – does early intensive SBP control (<140) changed outcomes vs standard of care (<180)?
- Borderline significance, but is safe
- Problem: meds used weren’t standardized across trial participants
- AHA 2015 guidelines: acute decrease in SBP to <140 safe
- ATACH-2 – SBP <140 vs <180 with standardized tx (Nicardipine)
- No difference in mortality
- Increased renal failure in <140 group in 1st 7 days
- Postulated to be due to the effect on auto regulation by chronic HTN
- Interact II – does early intensive SBP control (<140) changed outcomes vs standard of care (<180)?
- Anti-platelet reversal
- PATCH: platelet transfusion lead to increase in death + harm
- Problem: small study group
- PATCH: platelet transfusion lead to increase in death + harm
- Anticoagulation reversal
- INCH: INR (>2) reversal w 4 PCC – safe, effective (rapidly brings INR <2)
- Decreased early hematoma expansion
- INCH: INR (>2) reversal w 4 PCC – safe, effective (rapidly brings INR <2)
Ischemic stroke
- GOALS: 4.5h to tPA or 6h to thrombectomy
- Stent retrieval: 5 RCTs on IA & stent assisted clot retriever (NNT of 5)
- Criteria:
- Pre-stroke modified Rankin 0-1 (no deficits)
- tPA <4.5h since symptom onset
- ICA or prox MCA (M1) lesion
- Age ≥18
- NIHSS ≥6
- ASPECTS ≥ 6
- CT rating tool (early ischemia) to estimate risk of hemorrhagic transformation (low)
- W/in 6 hrs of symptom onset
- Criteria:
- MR CLEAN trial: general anesthesia negated endovascular benefit
- Poor outcome due to hypotension on induction?
- Goal: titrate conscious sedation to avoid movement and big BP changes
New trends in the field:
- 8-25% of CVA pts have unknown onset time
- Imaging (MRI) to look at tissue – i.e., MRI w DWI/FLAIR mismatch
- tPA for these patients? Thrombectomy? more RCTs upcoming
- MR-WITNESS – median time to tPA: 11h; safe (only 1.25% secondary ICH)
- Malignant MCA syndrome
- Swell early and require decompression (NNT 4 for modified Rankin <=3, NNT 2 for survival)
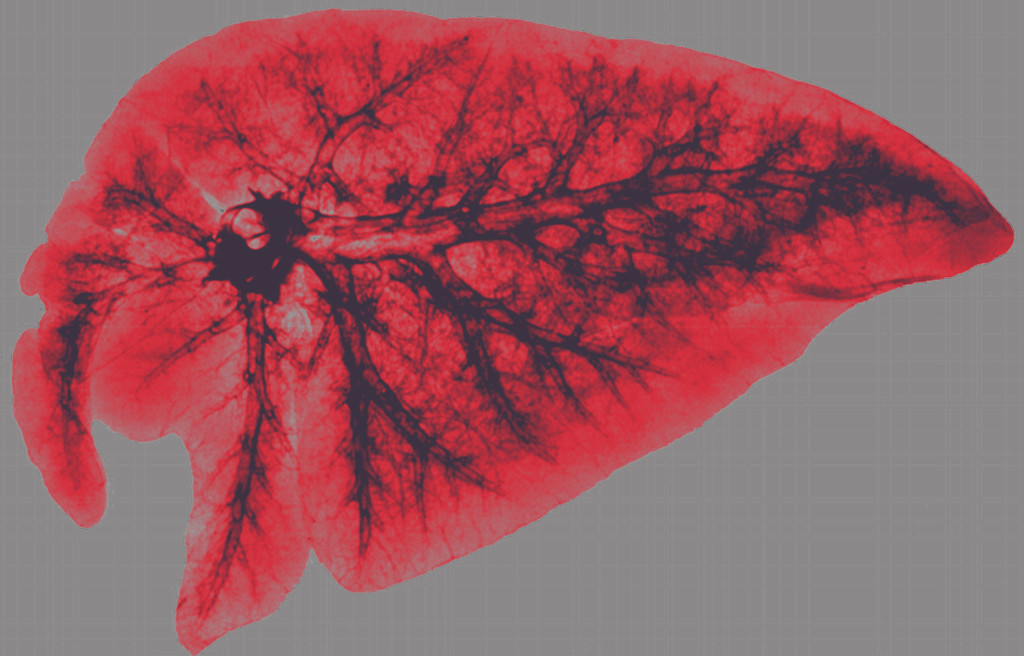
- SUR1-TRPM4 channel (rapid ATP depletion leads to opening of channel and increased intracellular water) blocked by Glyburide
- GAMES-RP trial – administration of glyburide did not avoid craniectomy but did show improvement in midline shift + biomarkers
Suggested Reading
- Qureshi AI, Palesch YY, Barsan WG, Hanley DF, Hsu CY, Martin RL, Moy CS, Silbergleit R, Steiner T, Suarez JI, Toyoda K, Wang Y, Yamamoto H, Yoon BW; ATACH-2 Trial Investigators and the Neurological Emergency Treatment Trials Network. Intensive Blood-Pressure Lowering in Patients with Acute Cerebral Hemorrhage. N Engl J Med. 2016 Jun 8. [NEJM Link]
- Andrews PJ, Harris BA, Murray GD. Hypothermia for Intracranial Hypertension after Traumatic Brain Injury. N Engl J Med. 2016 Apr 7;374(14):1385.[NEJM Link]
- Hemphill JC 3rd, Greenberg SM, Anderson CS, Becker K, Bendok BR, Cushman M, Fung GL, Goldstein JN, Macdonald RL, Mitchell PH, Scott PA, Selim MH, Woo D; American Heart Association Stroke Council; Council on Cardiovascular and Stroke Nursing; Council on Clinical Cardiology. Guidelines for the Management of Spontaneous Intracerebral Hemorrhage: A Guideline for Healthcare Professionals From the American Heart Association/American Stroke Association. Stroke. 2015 Jul;46(7):2032-60.[PubMed Link]
- Steiner T, Freiberger A, Griebe M, Hüsing J, Ivandic B, Kollmar R, Pfefferkorn T, Wartenberg KE, Weimar C, Hennerici M, Poli S. International normalised ratio normalisation in patients with coumarin-related intracranial haemorrhages–the INCH trial: a randomised controlled multicentre trial to compare safety and preliminary efficacy of fresh frozen plasma and prothrombin complex–study design and protocol. Int J Stroke. 2011 Jun;6(3):271-7.[PubMed Link]
- Rossetti AO, Rabinstein AA, Oddo A. Neurological prognostication of outcome in patients in coma after cardiac arrest. Lancet Neurol 2016; 15: 597–609. [The Lancet Link]
- Baharoglu MI, Cordonnier C, Al-Shahi Salman R, de Gans K, Koopman MM, Brand A, Majoie CB, Beenen LF, Marquering HA, Vermeulen M, Nederkoorn PJ, de Haan RJ, Roos YB; PATCH Investigators. Platelet transfusion versus standard care after acute stroke due to spontaneous cerebral haemorrhage associated with antiplatelet therapy (PATCH): a randomised, open-label, phase 3 trial. Lancet. 2016 Jun 25;387(10038):2605-13.[Pubmed Link]