Today we are very excited to host Dr. Lakhmir S. Chawla, nephrologist, intensivist, and international expert on the management of shock. Dr. Chawla has recently taken a sabbatical from his position as Professor of Critical Care Medicine, George Washington U to become the Chief Medical Officer of La Jolla Pharmaceuticals. It in this role he investigates an old and forgotten friend in the treatment of hypotension, and has become the chief researcher for the ATHOS (Angiotensin II for the Treatment of High-Output Shock) 3 trial. Today he takes a fascinating look at the way we treat shock-induced hypotension and asks one simple question: Can’t we do better?
Rules of Critical Care
Defend blood pressure
- “True” hypotension is an emergency
- MAP<65 needs attention IMMEDIATELY
- Hypotension → Decreased DBP → Decreased coronary blood flow → Cardiac ischemia → Decreased CO → Hypotension (repeat)
- Short durations hurt brain, kidneys, heart
- Longer durations of hypotension = worse outcomes
- Push dose, immediate fluids, etc.
- FIX IT!
- MAP<65 needs attention IMMEDIATELY
You MUST diagnose shock
- Always identify which type of shock!
- Stabilize/Defend BP
- Assessment of CO → Diagnose shock type
- Volume trial → Look for CO improvement
The choice of vasopressors is not always clear
- The case for Vasopressin>NE: VASST trials
- Are both studies underpowered? Is steroids+Vaso the magic solution for the truly sick?
- No consensus solution
- Are both studies underpowered? Is steroids+Vaso the magic solution for the truly sick?
- The comparison of NE to Dopa (SOAP II group)
- Poorly dosed Dopa in the comparison group (not studying the physiological rationale)
- NE may be better for you (for cardiogenic shock)
- Hypotension is due to a lack of catecholamines (just as HTN is due to an overabundance of them)
The time has come to look for alternative vasopressors
- Selepressin
- Vasopressin targets V1a, V1b for vasoconstriction
- Also targets Oxytocin and V2 → fluid overload and microvascular thrombosis
- Selepressin is a selective V1a agonist → targeted vasoconstriction
- Improves free water clearance (lacks V2 targeting) → less lung injury/less lung edema
- Less vascular leak (typical with Vasopressin)
- Vasopressin targets V1a, V1b for vasoconstriction
- Angiotensin II (Ang II)
- First trial: 1961, then disappeared
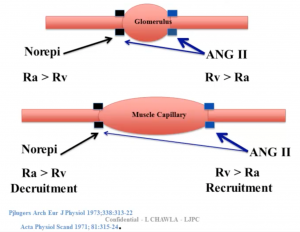
- Example: Distributive shock, s/p resuscitation, has INCREASED blood flow to kidneys → intraglomerular hypotension and AKI
- Treatment with Ang II leads to improvements
- NE leads to AFFERENT vasoconstriction
- Ang II → EFFERENT vasoconstriction (recruits capillary beds)
- Treatment with Ang II leads to improvements
- ATHOS trial
- Low doses of Ang II can cause catecholamine sparing
- 2 outliers had HYPERtension (due to ARDS?)
- Low doses of Ang II can cause catecholamine sparing
- SEVERE ARDS causes Ang II deficiency
- Pulmonary capillary endothelium damage can restrict conversion of Ang I to Ang II
- Ang II Pilot data conclusions
- IV Ang II has a role as a rescue vasopressor
- IV Ang II may be more useful in ARDS patients
- Currently undergoing a Phase III registration trial for Ang II as a vasopressor
- First FDA trial for a drug AS a vasopressor
Suggested Reading
- Chawla LS, Busse L, Brasha-Mitchell E, Davison D, Honiq J, Alotaibi Z, Seneff MG. Intravenous angiotensin II for the treatment of high-output shock (ATHOS trial): a pilot study. Crit Care. 2014 Oct 6;18(5):534.[PubMed Link]
- Russell JA, Walley KR, Singer J, Gordon AC, Hébert PC, Cooper DJ, Holmes CL, Mehta S, Granton JT, Storms MM, Cook DJ, Presneill JJ, Ayers D; VASST Investigators. Vasopressin versus norepinephrine infusion in patients with septic shock. N Engl J Med. 2008 Feb 28;358(9):877-87.[PubMed Link]
- Russell JA, Walley KR, Gordon AC, Cooper DJ, Hébert PC, Singer J, Holmes CL, Mehta S, Granton JT, Storms MM, Cook DJ, Presneill JJ; Dieter Ayers for the Vasopressin and Septic Shock Trial Investigators. Interaction of vasopressin infusion, corticosteroid treatment, and mortality of septic shock. Crit Care Med. 2009 Mar;37(3):811-8.[PubMed Link]