Today we welcome Josh D King, MD, Assistant Professor of Medicine at the University of Virginia School of Medicine where he also serves as the associate program director for the nephrology fellowship program. Dr. King is a rare specimen, with board certifications in both Nephrology and Toxicology he focuses on critical care nephrology, acute treatment of drug overdoses, and addressing acute poisoning and envenomation. In addition to his clinical work, Dr King is a prolific academician, publishing numerous journal articles on the topic of acute care toxicology. Today he was kind enough to travel up Interstate 95 and donate an hour of his time to explain what we HAVE TO KNOW if we plan to work in the modern ICU!
Clinical Pearls (Assisted by Dr. Shane Kappler)
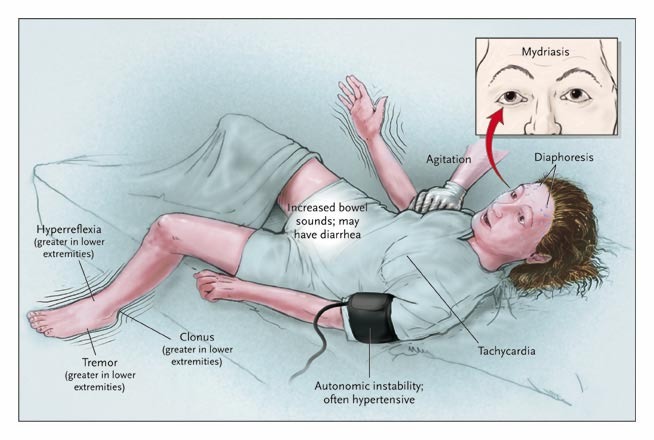
- Agitated Delirium: Sympathomimetic, Anticholinergic, and Serotonin syndrome
- General symptoms of tox induced agitated delirium
- Hypertension
- Tachycardia
- Mydriasis
- Hallucinations
- Paranoia
- Agitation
- Confusion
- Diaphoresis (less AC)
- Clonus/hyperreflexia (Serotonin)
- Which can all eventually lead down the common pathway of:
- Seizures
- Tachyarrhythmias
- Hyperthermia
- Rhabdomyolysis
- General symptoms of tox induced agitated delirium
- Novel drugs of abuse: “Novel psychoactive agents” aka NPAs
- Ex: Synthetic cannabinoids
- Primarily affects the CB1 receptor which induce serotonin, dopamine, NE release
- Symptoms:
- Largely sympathomimetic and serotonergic in nature (see above)
- Tremor, diaphoresis, HTN, tachcardia, mydriasis
- Hallucinations, agitation, delirim, paranoia
- Choreoform movements
- SEVERE effects:
- Uncoupling of oxidative phosphorylation → rhabdomyolysis, Sz, AKI, tachyarrhythmias, hyperthermia
- Vascular events: CVA, STEMI
- Non-resolving psychosis
- Testing for NPAs difficult secondary to unusual chemical structures and frequent changes by labs to stay ahead of regulations; will not show up on UDS
- Goals of patient management
- Control agitation
- Decrease sympathomimetic output
- Reduce serotonergic tone
- Address end organ toxicity
- Treatment
- GABA-A agonists, principally benzodiazepines
- IV fluids
- Antipsychotics for behavioral control
- Refractory seizures: benzos→ propofol→ barbiturates
- Avoid phenytoin, simply not effective
- Hyperthermia/uncoupling syndrome: GABA agonists, Dexmedetomidine as adjunct (not good for seizures)
- Hypertensive crisis: Vasodilators (nitro, nicardipine) and GABA agonists
- Avoid beta-blockers (uninterrupted alpha effect)
- Newer antidotes
- “Lipid sink”
- Isolates drugs outside of tissue
- Typically used for cardiogenic shock or arrest
- Usually intralipid; 1.5 ml/kg initially and 0.25 ml/kg/min x 15 minutes
- Used for lipophilic drugs
- Reasonable evidence for bupivacaine and has also been used for other local anesthetics
- “Scattered evidence” for cardiac sodium channel blockers (flecainide, TCAs, cocaine, diphenhydramine), CCBs, beta-blockers, antipsychotics
- Adverse effects:
- Pancreatitis, ARDS, AKI, and worsening shock
- Can interfere with CRRT and ECMO
- Isolates drugs outside of tissue
- Methylene blue
- Established role in methemoglobinemia
- Used in vasoplegia post cardiac surgery
- Potential use in refractory shock– makes less responsive to NO vasodilation through blocking guanidine cyclase activity (less cGMP)
- Scattered case reports and animal studies for CCBs, B-blocker, Amlodipine, septic shock, anaphylactic shock; unclear benefit although could be considered for salvage therapy
- Hydroxocobalamin
- Combines with CN to make vitamin B12
- Most frequently used for smoke inhalation/cyanide
- Evidence that it scavenges nitric oxide
- Case for cardiac surgery vasoplegia
- Animal models for Shock: septic, hemorrhagic, and cardiogenic
- Probably “not ready for prime time”
- Classified as salvage as last resort after lipids, methylene blue
- Can cause blood leak alarm on HD
- Combines with CN to make vitamin B12
- “Lipid sink”
Selected cases and key points
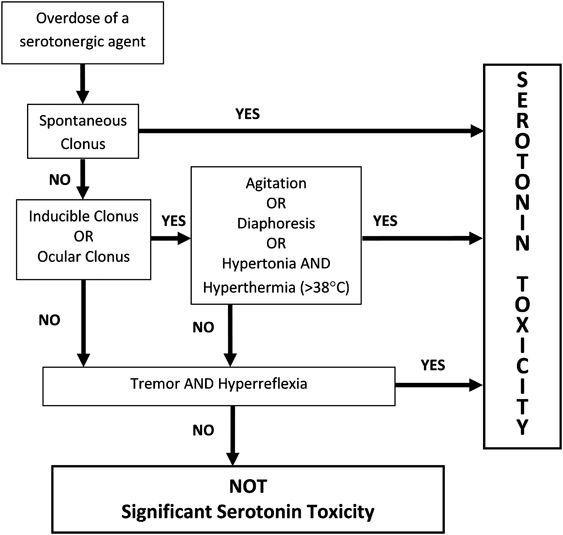
- Serotonin Syndrome
- Excessive stimulation of 5HT1a + 5HT2a receptors
- Hyperreflexia and clonus are pathognomonic (if not present consider other diagnosis)
- Serotonergic drugs:
- SSRIs, SNRIs, TCAs, other antidepressants (bupropion)
- Dextromethorphan, tramadol, meperidine, fentanyl, triptans
- MAOIs including linezolid and methylene blue, lithium
- Treatment
- Benzos, benzos, benzos (or propofol)
- Dexmedetomidine (as adjunct only)
- Cyproheptadine for mild cases (oral, can cloud picture)
- Excessive stimulation of 5HT1a + 5HT2a receptors
- Cefepime toxicity
- Cefepime crosses blood brain barrier, acts as GABA antagonist
- High levels→ renal failure
- Adverse effects:
- Myoclonus, encephalopathy, agitation, seizures, death
- Treatment
- Discontinuation, GABA agonists, hemodialysis
- Cefepime crosses blood brain barrier, acts as GABA antagonist
- Excipient toxicity
- Lorazepam and phenytoin dissolved in propylene glycol which is metabolized to lactic acid
- Bumetanide infusions can cause myalgias due to excipient
- Propofol-Related Infusion Syndromet
- Believed to be related to lipids in propofol compounded over prolonged, high-dose use.
- Can see refractory bradycardia/asystole, rhabdo, lactic acidosis, shock
- Extra fact: Ethylene glycol?
- Calculate “lactate gap”
- Some blood gas analyzers use lactate oxidase, which misreads glycolic acid (ethylene glycol metabolite) as lactic acid
- Calculate “lactate gap”
10 poisonings that scare me!
- Salicylates
- Danger of not recognizing patient acuity
- Buproprion XL formulations
- Risk fo late-onset szs
- Long-acting opioids
- Risk of resedation, must be watched carefully
- TCAs
- Danger of abrupt decompensation
- Baclofen
- Unrecognized withdrawal syndrome after overdose resolved
- CCBs
- Refractory hypotension
- INH
- Risk of refractory seizures
- CO
- Misdiagnosis
- HF acid (wheel cleansers)
- Acute torsades and/or V fib (QTc: 700-800)
- Any sedative-hypnotic (Baclofen, TCA, barbs)
- Misdiagnosis of brain death by clinical and EEG findings
Suggested Reading
- RTait RJ, Caldicott D, Mountain D, Hill SL, Lenton S. A systematic review of adverse events arising from the use of synthetic cannabinoids and their associated treatment. Clin Toxicol (Phila). 2016;54(1):1-13.[Pubmed Link]
- Gummin DD, Mowry JB, Spyker DA, Brooks DE, Fraser MO, Banner W. 2016 Annual Report of the American Association of Poison Control Centers’ National Poison Data System (NPDS): 34th Annual Report. Clin Toxicol (Phila). 2017 Dec;55(10):1072-1252.[Pubmed Link]
- Gosselin S, Hoegberg LC, Hoffman RS, Graudins A, Stork CM, Thomas SH, Stellpflug SJ, Hayes BD, Levine M, Morris M, Nesbitt-Miller A, Turgeon AF, Bailey B, Calello DP, Chuang R, Bania TC, Mégarbane B, Bhalla A, Lavergne V. Evidence-based recommendations on the use of intravenous lipid emulsion therapy in poisoning. Clin Toxicol (Phila). 2016 Dec;54(10):899-923.[Pubmed Link]