Today we welcome Zachary Kon, M.D., Assistant Professor in the Department of Cardiothoracic Surgery at NYU. In addition to acting as the Surgical Director of Pulmonary Hypertension/Pulmonary Thromboendarterectomy Program, Dr. Kon also acts as the Surgical Director of the NYU Lung Transplantation Program. In addition to > 70 peer-reviewed publications, he has been invited all over the world as an expert speaker in the field pulmonary embolism therapy. We are fortunate to have him in-house to share his knowledge of what to do when the PE is starting to become overwhelming!
Clinical Pearls
- Massive PE is defined by HD instability
- It is the HD compromise, not the hypoxia, that leads to morbidity/mortality
- Surgical embolectomy has become a mainstay of treatment (mortality as low as 5-10%)
- Intubation worsens mortality!
- Submassive PE is HD stable with RV strain/dysfunction (TTE, CT scan, troponin/BNP)
- VA-ECMO use has facilitated decompression of the right heart and improved outcomes
- Potential triage of patients who would benefit from embolectomy
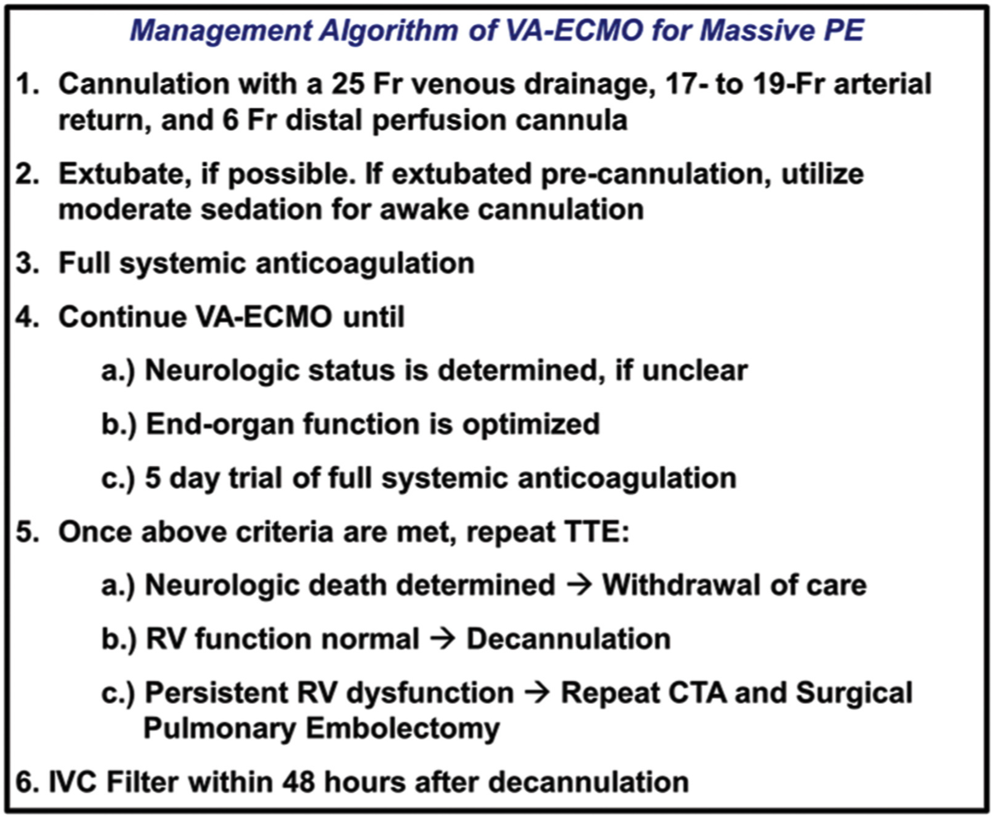
- Algorithm: ECMO is initial strategy to recover organ function and either wean to survival, embolectomy, or to withdrawal of care.
- Decreased mortality (3% vs. 23%), decreased time from arrest to intervention (4 hrs vs. 11.5 hrs), and decreased need for surgical embolectomy (55% vs. 100%)
- Potential triage of patients who would benefit from embolectomy
The Annals of Thoracic Surgery 2018 105, 498-504
-
- RV recovery on VA-ECMO dictated by:
- History of prior PE
- Chronic DVT (> 2 weeks)
- Higher BNP on presentation (not troponin!)
- RV recovery on VA-ECMO dictated by:
- Fallacies
- Too peripheral
- Distal, sub-segmental vessels can be accessed and removed
- Too invasive
- Minimally invasive approaches (5-7 cm incisions) can be used with excellent outcomes
- Hospital LOS: 4 days
- Minimally invasive approaches (5-7 cm incisions) can be used with excellent outcomes
- Can’t rehabilitate
- Cannulation does NOT require intubation
- All non-intubated ECMO pts can mobilize
- Too peripheral
- Random facts to know!
- Anatomic distribution or burden of clot DOES NOT correlate to clinical outcomes
- Chronic thromboembolic pulm HTN (CTEP) risk is 3%, though 5-10x the risk when presenting with pulm HTN + acute PE!
- Submassive PE + simple AC = > 50% risk for CTEP vs > 15% with thrombolysis (MOPETT)
- As PA pressure continues to increase, mortality worsens
Suggested Reading
- Konstantinides SV, Vicaut E, Danays T, Becattini C, Bertoletti L, Beyer-Westendorf J, Bouvaist H, Couturaud F, Dellas C, Duerschmied D, Empen K, Ferrari E, Galiè N, Jiménez D, Kostrubiec M, Kozak M, Kupatt C, Lang IM, Lankeit M, Meneveau N, Palazzini M, Pruszczyk P, Rugolotto M, Salvi A, Sanchez O, Schellong S, Sobkowicz B, Meyer G. Impact of Thrombolytic Therapy on the Long-Term Outcome of Intermediate-Risk Pulmonary Embolism. J Am Coll Cardiol. 2017 Mar 28;69(12):1536-1544.[Pubmed Link]
- Kalra R, Bajaj NS, Arora P, Arora G, Crosland WA, McGiffin DC, Ahmed MI. Surgical Embolectomy for Acute Pulmonary Embolism: Systematic Review and Comprehensive Meta-Analyses. Ann Thorac Surg. 2017 Mar;103(3):982-990.[Pubmed Link]
- Kuo WT, Banerjee A, Kim PS, DeMarco FJ Jr, Levy JR, Facchini FR, Unver K, Bertini MJ, Sista AK, Hall MJ, Rosenberg JK, De Gregorio MA. Pulmonary Embolism Response to Fragmentation, Embolectomy, and Catheter Thrombolysis (PERFECT): Initial Results From a Prospective Multicenter Registry. Chest. 2015 Sep;148(3):667-673. [Pubmed Link]
- Piazza G, Hohlfelder B, Jaff MR, Ouriel K, Engelhardt TC, Sterling KM, Jones NJ, Gurley JC, Bhatheja R, Kennedy RJ, Goswami N, Natarajan K, Rundback J, Sadiq IR, Liu SK, Bhalla N, Raja ML, Weinstock BS, Cynamon J, Elmasri FF, Garcia MJ, Kumar M, Ayerdi J, Soukas P, Kuo W, Liu PY, Goldhaber SZ; SEATTLE II Investigators. A Prospective, Single-Arm, Multicenter Trial of Ultrasound-Facilitated, Catheter-Directed, Low-Dose Fibrinolysis for Acute Massive and Submassive Pulmonary Embolism: The SEATTLE II Study. JACC Cardiovasc Interv. 2015 Aug 24;8(10):1382-92.[Pubmed Link]