Today we are fortunate to welcome Sam Hsu, MD, RDMS, Assistant Professor for the University of Maryland Medical School. Dr. Hsu is the acting Emergency Department Ultrasound Director at one of the UMMC satellite centers her in Baltimore, Mercy Medical Center. He also takes on command of medical student emergency ultrasound education for the medical school. I guess you could say, he lives and breaths ED ultrasound! Today he takes us through his algorithm on how to approach ultrasonography of the lungs. I have attending many lectures on the topic and have even performed lung US research, but this lecture is the best presentation I have ever seen on the topic. You NEED to watch this lecture.
Podcast: Play in new window | Download
Subscribe: Apple Podcasts | RSS
Clinical Pearls – assisted by Dr. Shane Kappler
- Core Lung US concepts:
- Air reflects 99% of the US beam
- Aeration prevents true images of lung → normal lungs are never imaged
- “Healthy lungs are hidden”; “sick lungs can be seen”
- Probes are also acoustic mirrors creating an “infinate mirror”
- Images will degrade with time…
- Aeration prevents true images of lung → normal lungs are never imaged
- Air behind a smooth surface (pleura, diaphragm) creates an acoustic mirror
- Air reflects 99% of the US beam
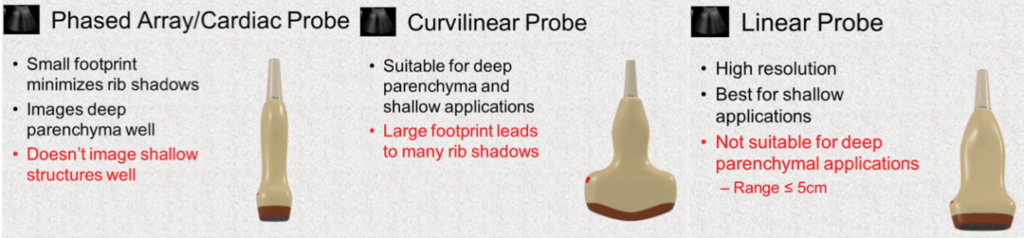
- Probe selection is important:
- Recognize normal, after that ABnormal is obvious
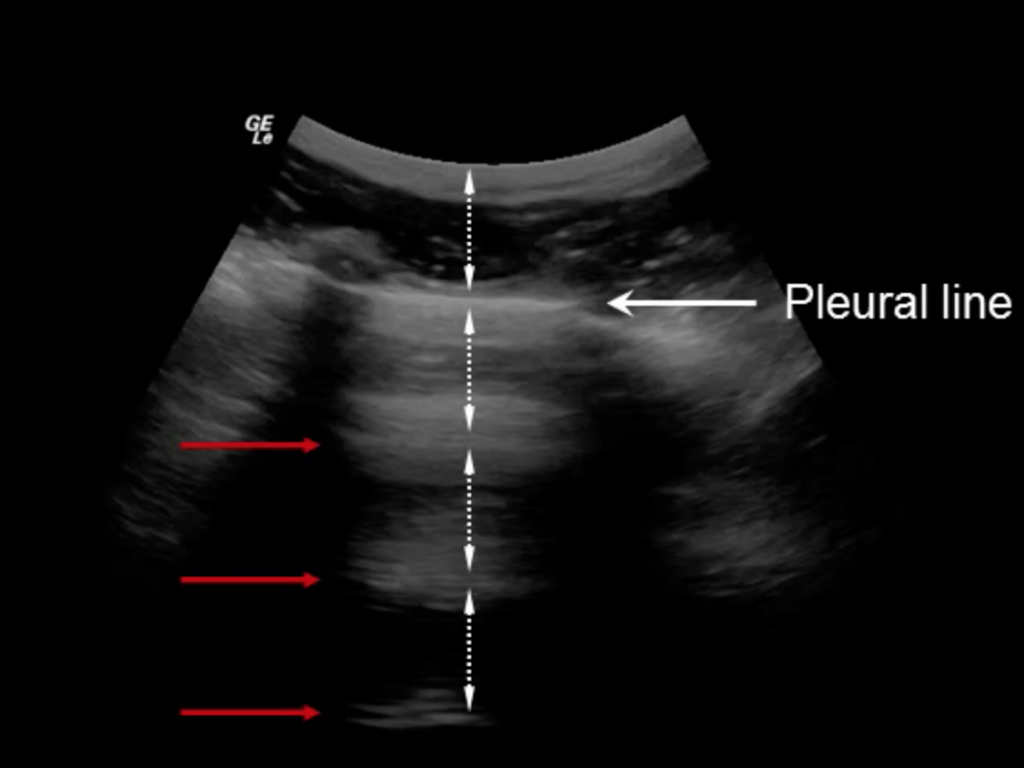
- A-lines: horizontal and normal
- hyper-echoic and represent “reverberation” artifact
- Spacing approximates distance from probe to pleura
- hyper-echoic and represent “reverberation” artifact
- A-lines: horizontal and normal
-
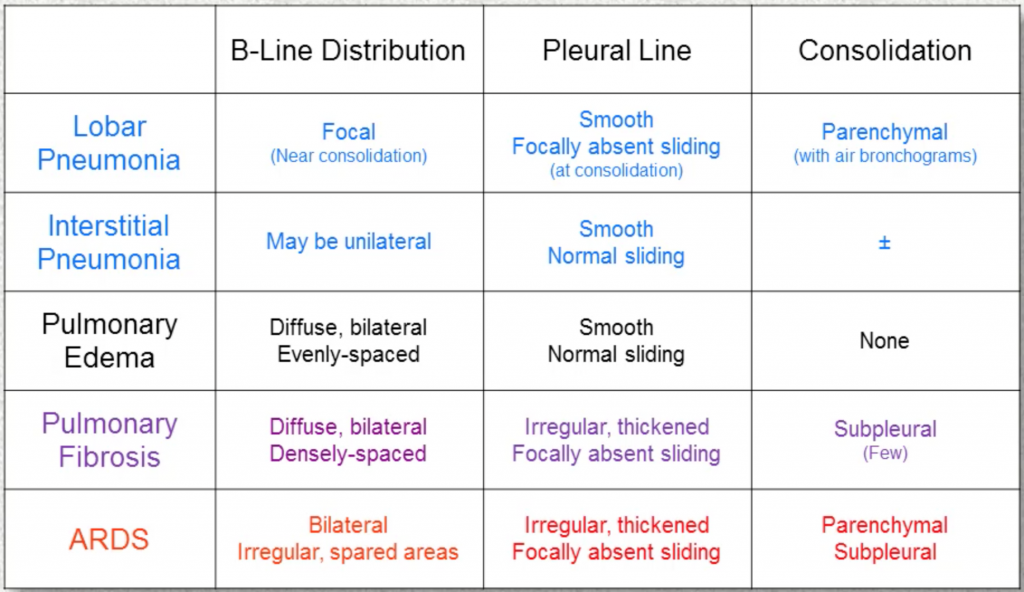
- B-lines: vertical and can be ABnormal (≥3 per rib interspace)
- Hyper-echoic, comet-tail
- Extends to BOTTOM of screen
- Arise from and move with visceral pleura
- Erase A-lines
- Hyper-echoic, comet-tail
- B-lines: vertical and can be ABnormal (≥3 per rib interspace)
-
- Z-lines: vertical, non-diagnostic
- Arise from parietal pleura (don’t slide)
- Do not reach the bottom
- Do not erase A-lines
- Normal AND abnormal lung
- Arise from parietal pleura (don’t slide)
- Z-lines: vertical, non-diagnostic
- Parenchymal findings
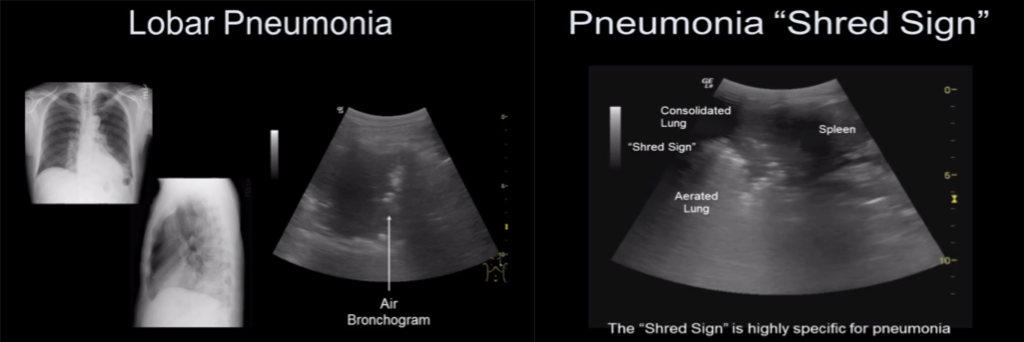
- Consolidation eval, need evals of ALL lung fields
- Hypo-density with hyper-echoic material (air bronchogram)
- Shred sign: Interface btw consolidated lung and normal lung (ragged edge)
- Very sensitive when compared to CT scan (adults) or CXR (peds)
- No A-lines or B-lines within consolidation
- Hypo-density with hyper-echoic material (air bronchogram)
- Consolidation eval, need evals of ALL lung fields
-
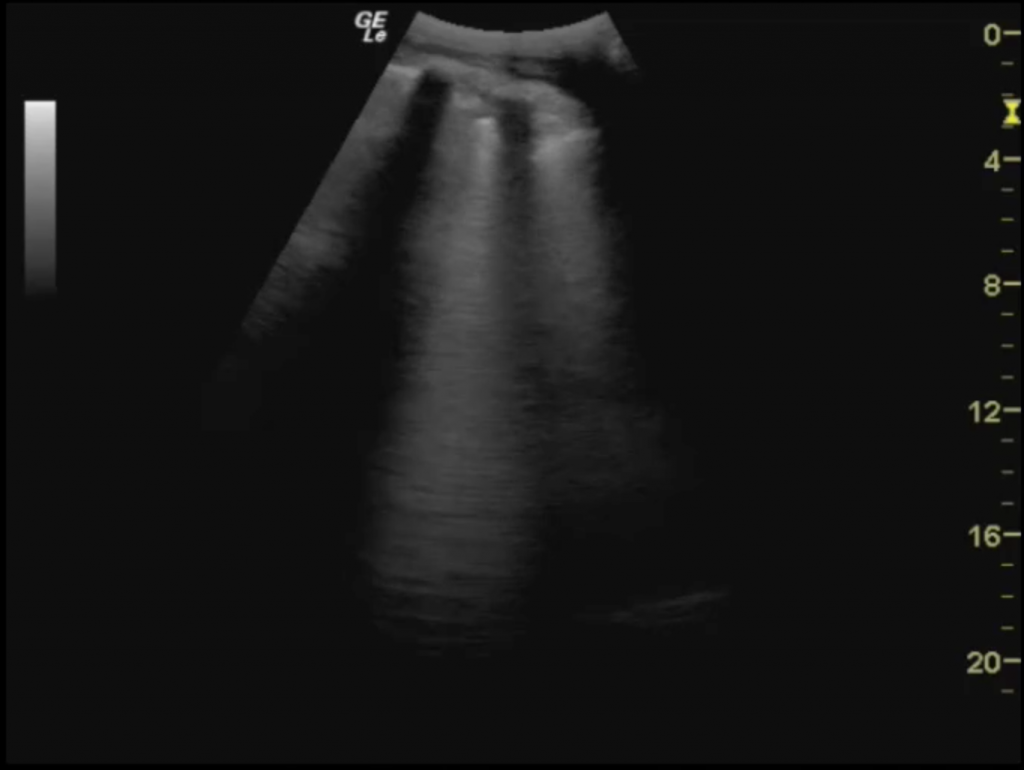
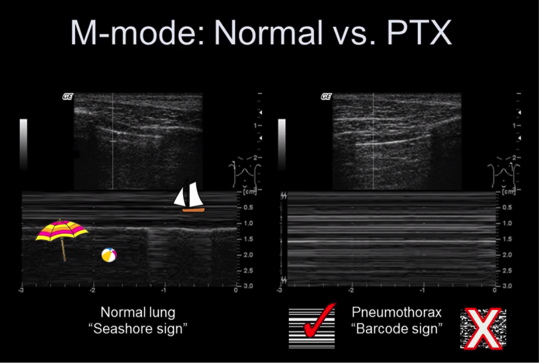
- Pneumothorax (PTX)
- Orient probe longitudinally and look for “lung sliding”
- Image most anterior part of chest + image several interspaces
- Rules in: lung point, M-mode “barcode” sign
- Rules out: pleural sliding B-lines, lung pulse, M-mode “seashore” sign
- Can see A-lines and Z-lines wth a PTX
- Orient probe longitudinally and look for “lung sliding”
- Pneumothorax (PTX)
-
-
-
- CAUTION: M-mode not reliable in labored breathing, lung bulla, cavities or severe emphysema/COPD
- Use a linear probe, adjust depth so pleura is centered and look for sliding, study M-mode closely
- CAUTION: M-mode not reliable in labored breathing, lung bulla, cavities or severe emphysema/COPD
- Lung pulse: Heart beats transmitted through the lung; it looks like how it sounds (using m-mode to find pulse below)
- Rules out a PTX
-
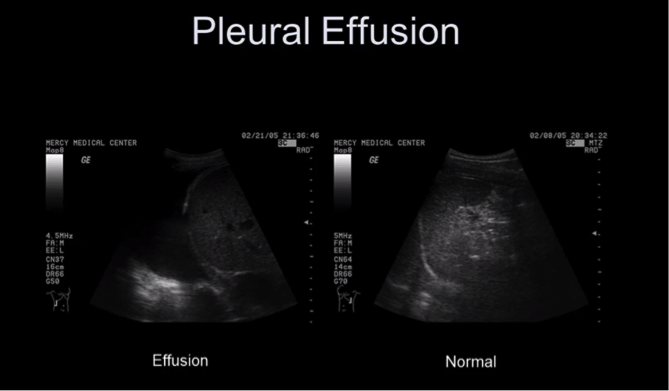
- Pleural effusion
- US can detect as little as 20cc of fluid
- Use curvilinear or phased array probe; place probe posterior/inferior
- Anechoic, above the diaphragm
- US can detect as little as 20cc of fluid
-
- Diaphragm evaluation
- Thickness: Linear probe, coronal plane (pointer towards head), mid-axillary line, caudal enough to view liver/spleen
- You would want to measure “thickening fraction“: (Inspiratory-expiratory)/Expiratory
- Normal TF> 30-36% (normal spontaneous breathing)
- Less = failure to wean
- Average expiratory thickness 1.7mm (thinner suggest atrophy)
- Caveat: probe resolution is ~0.1mm with a 5-7% error rate
- Normal TF> 30-36% (normal spontaneous breathing)
- You would want to measure “thickening fraction“: (Inspiratory-expiratory)/Expiratory
- Excursion: Curved probe, lateral to mid-clvicular line (pointer towards head), rock probe cephalad
- M-mode, perpendicular to diaphragm, with measurement
- Normal > 10-14 mm (spont breath)
- > 25 mm (max insp effort)
- M-mode, perpendicular to diaphragm, with measurement
- Thickness: Linear probe, coronal plane (pointer towards head), mid-axillary line, caudal enough to view liver/spleen
Suggested Reading
- Nazerian P, Volpicelli G, Vanni S, Gigli C, Betti L, Bartolucci M, Zanobetti M, Ermini FR, Iannello C, Grifoni S. Accuracy of lung ultrasound for the diagnosis of consolidations when compared to chest computed tomography. Am J Emerg Med. 2015 May;33(5):620-5.[Pubmed Link]
- Zambon M, Greco M, Bocchino S, Cabrini L, Beccaria PF, Zangrillo A. Assessment of diaphragmatic dysfunction in the critically ill patient with ultrasound: a systematic review. Intensive Care Med. 2017 Jan;43(1):29-38.[Pubmed Link]
- Lichtenstein DA, Mezière G, Lascols N, Biderman P, Courret JP, Gepner A, Goldstein I, Tenoudji-Cohen M. Ultrasound diagnosis of occult pneumothorax. Crit Care Med. 2005 Jun;33(6):1231-8.[Pubmed Link]