Please welcome back an old friend of Baltimore, Karen G. Hirsch, MD. Dr. Hirsch is an Assistant Professor of Neurology and the Director of Neurocritical Care at the Stanford University Medical Center. She is also one of the guru’s and experts in the field of neuroprognostication after cardiac arrest leading to a multitude of publications and numerous grants. Today we are exceedingly fortunate to have her grace the halls of The University of Maryland to give us a crash course on what we SHOULD be doing for our cardiac arrest patients. I assure you, this is a lecture all of us need to hear!
Podcast: Play in new window | Download
Subscribe: Apple Podcasts | RSS
Clinical Pearls (Assistance by Dr. Kamel Gharaibeh)
- Epidemiology
- Over 500,000 cases of cardiac arrest per year in USA (75% are out of hospital)
- Up to 60% of those with ROSC ultimately “survive”, but with significant functional limitations & ~80% remain comatose
- 60-80% of patients who survive ROSC die from withdrawal of care due to neurologic status
- Post-cardiac arrest syndrome
- Focus has changed from cardio-pulmonary resuscitation to cardio-cerebral resuscitation
- De-emphasize ventilation & focus on cardiac and cerebral perfusion
- Minimize ischemia-reperfusion injury leading to morbidity
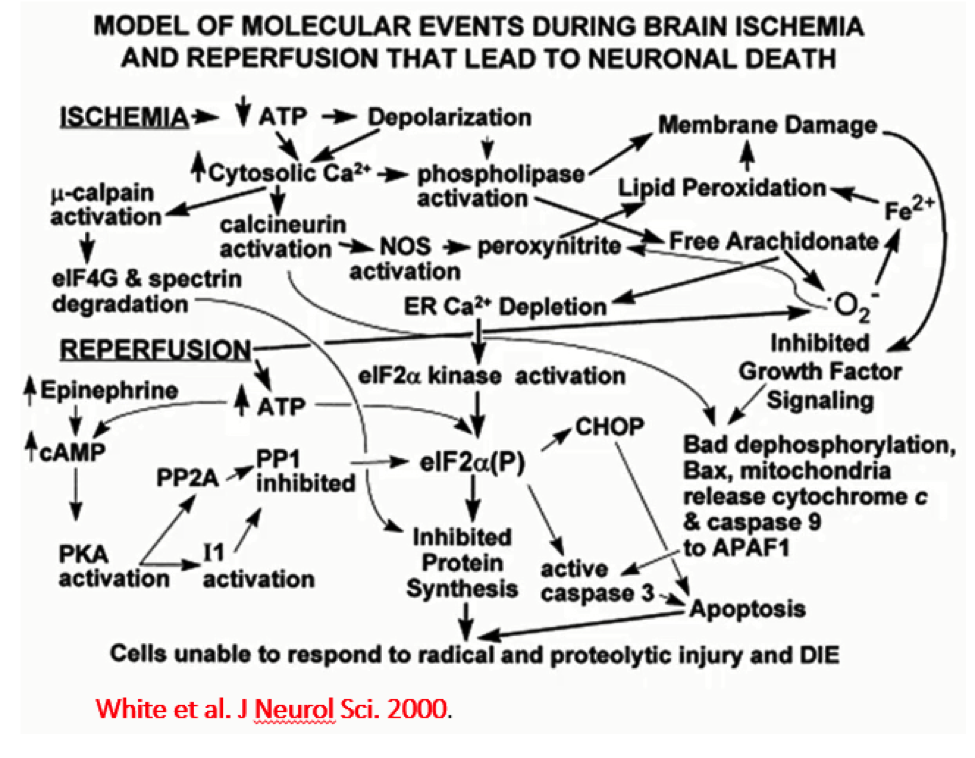
- Pathophysiology
- Complex but includes global ischemia (no flow) → global hypoperfusion (low flow) → gross reperfusion (reperfusion):
- Critical care management
- Regional systems of care
- Balance transport time with clinical expertise
- Early goal-directed therapy with hemodynamic optimization
- Therapeutic hypothermia vs. TTM
- Early intervention to address underlying cause
- Regional systems of care
- Hemodynamics after cardiac arrest
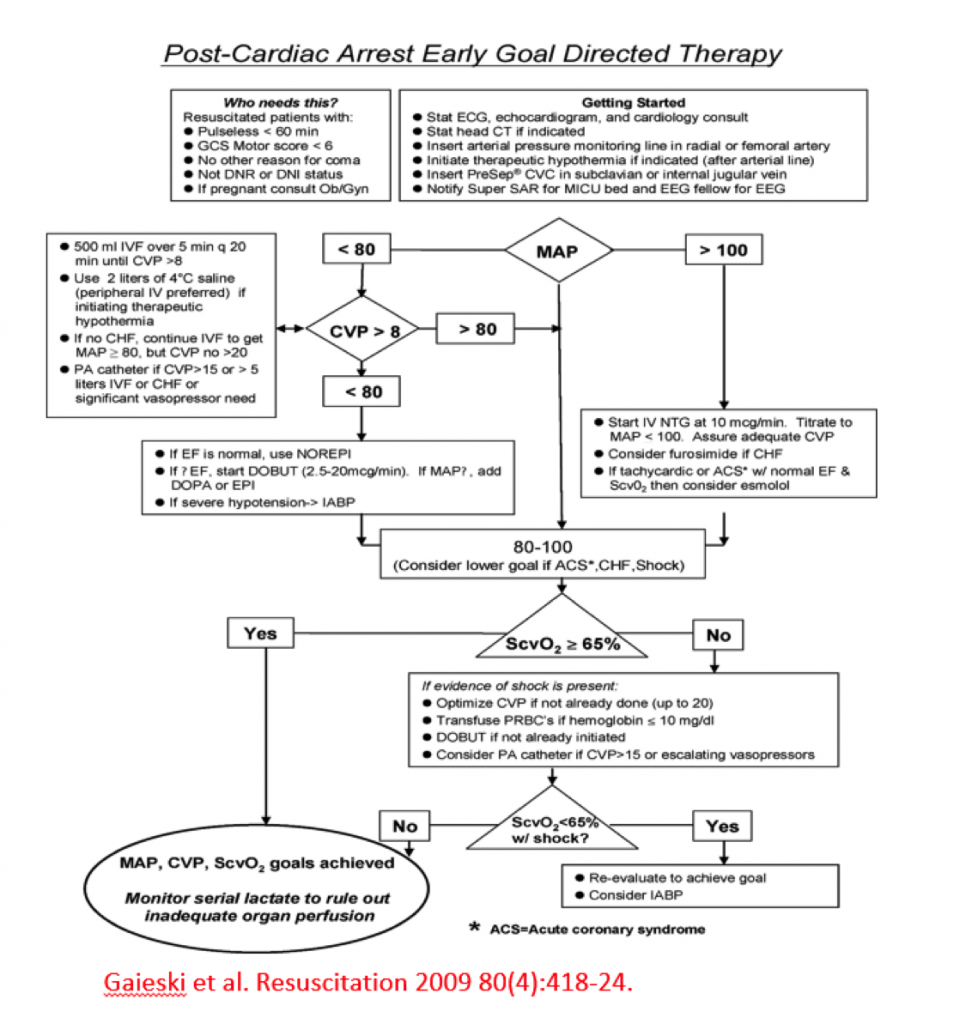
- Early goal-directed therapy
- The problem with algorithm (see below) is that it does not include neuromonitoring – not guided by cerebral pressure perfusion
- Among patients requiring vasopressors, combined vasopressin-methylprednisolone-epinephrine (VSE) during CPR, and stress-dose hydrocortisone in post-resuscitation shock, (compared with epinephrine/saline placebo) resulted in improved survival to hospital discharge with favorable neurological status (JAMA)
- Patients in VSE group had a higher blood pressure and higher SVO2 (both significant), which may have affected the results
- A prospective observation analysis showed that time-weighted average MAP (70-90 mmHg) was associated with good neurologic outcome (Crit Care Med)
- Outcome measures
- Still uncertain for the EXACT measure to determine neurological outcome.
- Early goal-directed therapy
- Therapeutic Hypothermia
- OHCA:
- 2002: In patients with ROSC s/p V-fib arrest, therapeutic mild hypothermia increased favorable neurologic outcome & reduced mortality. However, some of the normothermic group was actually hyperthermic, which could have affected the results. (NEJM)
- 2013: TTM trial showed in unconscious survivors of out-of-hospital cardiac arrest of presumed cardiac cause, hypothermia at a targeted temperature of 33°C did not confer a benefit as compared with a targeted temperature of 36°C (NEJM)
- IHCA:
- 2016: Cohort study showing TTM led to a lower chance of both survival AND survival with good neuro outcome, need RCT (JAMA)
- Guidelines still recommend maintaining a constant temperature between 32oC-36oC during TTM x 24 hours
- Ongoing trials:
- New TTM-2 trial is looking at 33oC vs < 37.5oC
- ICE-CAP Trial → assessing influence of cooling duration on efficacy in cardiac arrest patients
- OHCA:
- Prognostication
- We should never talk about prognosis in the first 24 hours after cardiac arrest
- Premature documentation of poor prognosis may contribute to early decisions to withdraw care
- Some clinical features should be interpreted with more caution after cardiac arrest:
- EEG background reactivity is useful in determining the prognosis after CA treated with therapeutic hypothermia
- Motor response, brainstem reflexes, myoclonus, absent pupil & corneal reflexes are unreliable prognostic measures, especially in the first 24 hours
- Some patients with extensor posturing had a good outcome
- Clinical examination (i.e., brainstem reflexes, motor response, presence of myoclonus) at day #3 after cardiac arrest remains an accurate predictor of outcome after therapeutic hypothermia (Ann Neurol)
- Sedative medications in both hypothermic and non-hypothermic patients may confound the clinical exam
- MRI is not very helpful in first 24 hours
- It is helpful on day #2 to day #5.
- In the absence of clear guidance from patient/surrogate, irreversible management decisions should not be made on the basis of a single parameter or early in the clinical course
- Potential Algorithm (presented by Dr. Hirsch):
- We should never talk about prognosis in the first 24 hours after cardiac arrest
Suggested Reading
- Chan PS, Berg RA, Tang Y, Curtis LH, Spertus JA; American Heart Association’s Get With the Guidelines–Resuscitation Investigators. Association Between Therapeutic Hypothermia and Survival After In-Hospital Cardiac Arrest. JAMA. 2016 Oct 4;316(13):1375-1382. [Pubmed Link]
- Nielsen N, Wetterslev J, Cronberg T, Erlinge D, Gasche Y, Hassager C, Horn J, Hovdenes J, Kjaergaard J, Kuiper M, Pellis T, Stammet P, Wanscher M, Wise MP, Åneman A, Al-Subaie N, Boesgaard S, Bro-Jeppesen J, Brunetti I, Bugge JF, Hingston CD, Juffermans NP, Koopmans M, Køber L, Langørgen J, Lilja G, Møller JE, Rundgren M, Rylander C, Smid O, Werer C, Winkel P, Friberg H; TTM Trial Investigators. Targeted temperature management at 33°C versus 36°C after cardiac arrest. N Engl J Med. 2013 Dec 5;369(23):2197-206. [Pubmed Link]
- Rittenberger JC, Callaway CW. Temperature management and modern post-cardiac arrest care. N Engl J Med. 2013 Dec 5;369(23):2262-3. [Pubmed Link]