Justin Richards, MD, Assistant Professor and Fellowship & Education Director, Division of Trauma Anesthesiology at the University of Maryland SOM, presents the weekly multi-departmental critical care fellows’ lecture on “Plasma Based Resuscitation: Should we pamper our critically ill patients?”
Summary by Dr. Jason Nam
Introduction
Plasma can be used as a resuscitation fluid. The PAMPer study titled Prehospital Plasma during Air Medical Transport in Trauma Patients at Risk for Hemorrhagic Shock. looked at injured patients at risk for hemorrhagic shock. In this study, the prehospital administration of thawed plasma was safe and resulted in lower 30-day mortality and a lower median prothrombin-time ratio than standard-care resuscitation.
What is plasma?
- Plasma is coming from blood donation. RBCs spun off. Plasma is the yellow fluid. Thawed plasma can be used for up to 5 days. Plasma constitutes most of the intravascular volume. Mostly water. Hyper-natremic. Has all the coagulation factors. Fibrinogen. Even some anticoagulants.
- Plasma has compatibility concerns. RBC universal recipient is AB positive. Universal plasma donor is AB. Problem with AB plasma is that it is 4% of population. Next acceptable plasma is type A.
How do we know type A plasma is safe?
- Safety of the use of group A plasma in trauma: the STAT study.
- An even larger study. No difference in outcome. Incompatible type A plasma transfusion in patients requiring massive transfusion protocol: Outcomes of an Eastern Association for the Surgery of Trauma multicenter study.
Let’s look at studies that assess the use of plasma in massive resuscitation.
- This first study shows no effectiveness in plasma use. RCT shows no survival benefit. Plasma-first resuscitation to treat haemorrhagic shock during emergency ground transportation in an urban area: a randomised trial.
- However, retrospective study after retrospective study shows benefits of early use of increased plasma.
- And then we arrive at the landmark PROPPR trial. Transfusion of plasma, platelets, and red blood cells in a 1:1:1 vs a 1:1:2 ratio and mortality in patients with severe trauma: the PROPPR randomized clinical trial. Rationale of high ratios of plasma to RBCs. There is increasing evidence of plasma use in resuscitation.
Why does plasma use make sense? Does it make sense?
- Trauma causes an acute disruption of the equilibrium between all components of hemostasis. Patients with a combination of severe tissue damage and systemic hypoperfusion will progress rapidly to an endogenous coagulopathy (Acute traumatic coagulopathy)
What does plasma do?
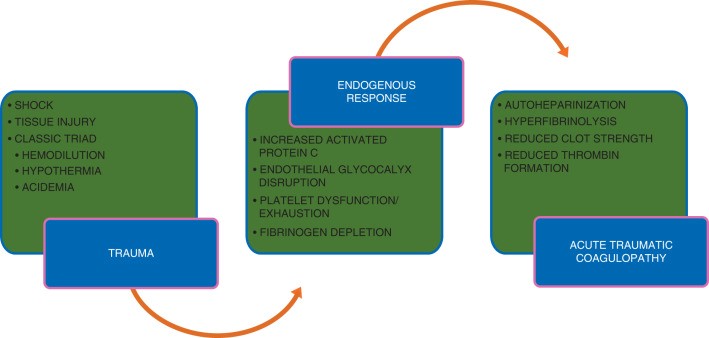
FFP can help with fibrinogen depletion and thrombin formation.
Other points
- Combat trial. No significant differences seen in mortality. Plasma-first resuscitation to treat haemorrhagic shock during emergency ground transportation in an urban area: a randomised trial.
- Should we give prehospital plasma? Maybe a difference in transit times for the two studies? We don’t know how they are resuscitated once they get to hospital. Penetrating vs. blunt trauma? Air vs. ground transportation?
- Would it work in sepsis?
- In sepsis, you lose the endothelial glycocalyx. You lose barrier function. You have capillary leak.
- Plasma was used to guide resuscitation in a rat model for sepsis. Plasma Resuscitation Improved Survival in a Cecal Ligation and Puncture Rat Model of Sepsis. Plasma-infused rats had improved mortality. Restoring endothelial glycocalyx is very important.
- Probable next research area. Potential role for plasma resuscitation outside of hemorrhage.
References
Moore, Hunter B., et al. “Plasma-first resuscitation to treat haemorrhagic shock during emergency ground transportation in an urban area: a randomised trial.” The Lancet 392.10144 (2018): 283-291. https://www-ncbi-nlm-nih-gov.proxy-hs.researchport.umd.edu/pubmed/30032977
Kozar, Rosemary A., et al. “Plasma restoration of endothelial glycocalyx in a rodent model of hemorrhagic shock.” Anesthesia and analgesia112.6 (2011): 1289. https://www-ncbi-nlm-nih-gov.proxy-hs.researchport.umd.edu/pubmed/21346161
Sperry, Jason L., et al. “Prehospital plasma during air medical transport in trauma patients at risk for hemorrhagic shock.” New England Journal of Medicine 379.4 (2018): 315-326. https://www-ncbi-nlm-nih-gov.proxy-hs.researchport.umd.edu/pubmed/30044935
Uploaded by Sami Safadi, MD