Brain Injury after Cardiac Arrest: Management, Prognosis and Controversies
Summary written by Dr. Kamel Gharaibeh
Epidemiology
- Over 500,000 cases of cardiac arrest per year in USA (75% are out of hospital)
- Most morbidity & mortality in those with ROSC results from neurologic injury
- 60-80% of patients who survive ROSC die from withdrawal of care due to neurologic status
- Up to 60% of those with ROSC ultimately survive, but with significant functional limitations & ~80% remain comatose
Post-cardiac arrest syndrome
- Focus has changed from cardio-pulmonary resuscitation to cardio-cerebral resuscitation
- De-emphasize ventilation & focus on cardiac and cerebral perfusion
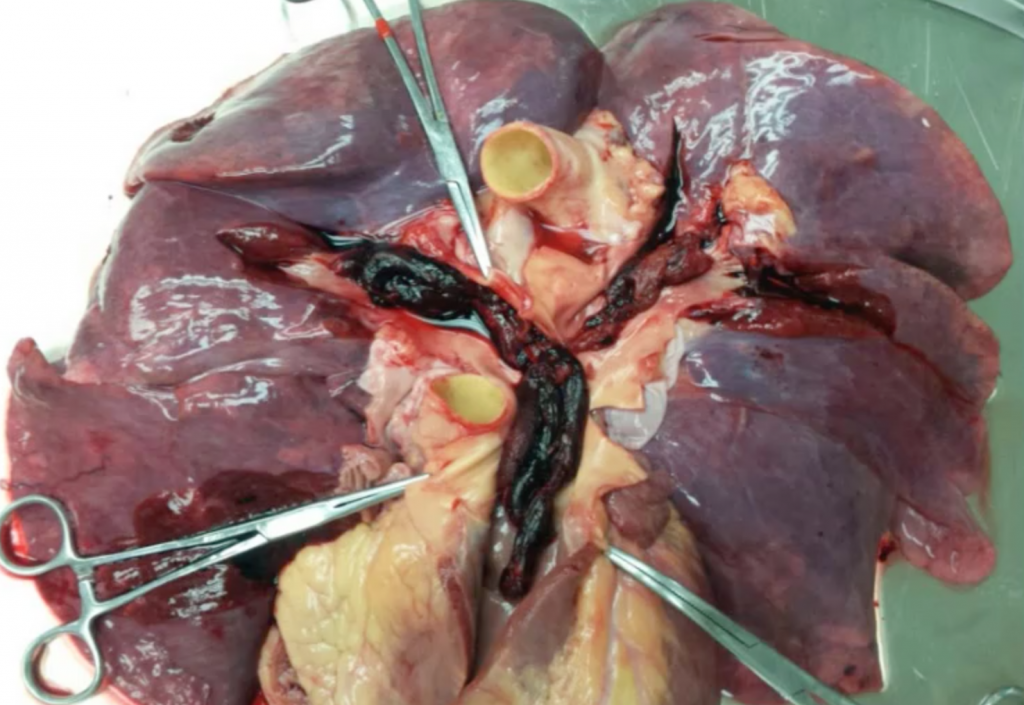
Pathophysiology
- Complex but includes global ischemia (no flow) à global hypoperfusion (low flow) à gross reperfusion (reperfusion)
Critical care management
- Regional systems of care – balance transport time with clinical expertise
- Early goal-directed therapy with hemodynamic optimization
- Therapeutic hypothermia
- Early intervention to address underlying cause
Hemodynamics after cardiac arrest
- Early goal-directed therapy
- The problem with algorithm is that it does not include neuromonitoring – not guided by cerebral pressure perfusion
- Among patients with cardiac arrest requiring vasopressors, combined vasopressin-methylprednisolone-epinephrine (VSE) during CPR, and stress-dose hydrocortisone in post-resuscitation shock, (compared with epinephrine/saline placebo) resulted in improved survival to hospital discharge with favorable neurological status; however, patients in VSE group had a higher blood pressure and higher SVO2, which may have affected the results. (Mentzelopoulos et al. JAMA 2013)
- A prospective observation analysis showed that time-weighted average MAP was associated with good neurologic outcome at a threshold of MAP >70mmHg (Kilgannon et al. CCM in 2014)
Therapeutic Hypothermia
- In patients with ROSC s/p V-fib arrest, therapeutic mild hypothermia increased favorable neurologic outcome & reduced mortality. However, some of the normothermic group was actually hyperthermic, which could have affected the results. (NEJM 2002)
- TTM trial showed in unconscious survivors of out-of-hospital cardiac arrest of presumed cardiac cause, hypothermia at a targeted temperature of 33°C did not confer a benefit as compared with a targeted temperature of 36°C (Nielsen et al., NEJM 2013)
- Guidelines recommend maintaining a constant temperature between 32oC-36oC during TTM
- TTM-2 trial is looking at 33oC vs < 37.5oC
- ICE-CAP Trial à assessing influence of cooling duration on efficacy in cardiac arrest patients
Prognostication
- We should never talk about prognosis in the first 24 hours after cardiac arrest. Premature documentation of poor prognosis may contribute to early decisions to withdraw care.
- Some clinical features should be interpreted with more caution after cardiac arrest. EEG background reactivity is useful in determining the prognosis after CA treated with therapeutic hypothermia.
- Motor response, brainstem reflexes, myoclonus, absent pupil & corneal reflexes are unreliable prognostic measures, especially in the first 24 hours. Some patients with extensor posturing had a good outcome.
- Clinical examination (i.e., brainstem reflexes, motor response, presence of myoclonus) at day #3 after cardiac arrest remains an accurate predictor of outcome after therapeutic hypothermia (Fugate et al, Ann Neurol 2010). Sedative medications in both hypothermic and non-hypothermic patients may confound the clinical exam.
- MRI is not very helpful in first 24 hours. It is helpful on day #2 to day #5.
- In the absence of clear guidance from patient/surrogate, irreversible management decisions should not be made on the basis of a single parameter or early in the clinical course.
Though not perfect, the Outcome Algorithm should look something like this
References
- White BC, Sullivan JM, DeGracia DJ, et al. Brain ischemia and reperfusion: molecular mechanisms of neuronal injury. J Neurol Sci. 2000; 179(1-2):1-33.
- Gaieski DF, Band RA, Abella BS, et al. Early goal-directed hemodynamic optimization combined with therapeutic hypothermia in comatose survivors of out-of-hospital cardiac arrest. Resuscitation. 2009; 80(4):418-24.
- Mentzelopoulos SD, Malachias S, Chamos C, et al. Vasopressin, steroids, and epinephrine and neurologically favorable survival after in-hospital cardiac arrest: a randomized clinical trial. JAMA. 2013 Jul 17; 310(3):270-9
- Kilgannon JH, Roberts BW, Jones AE, et al. Arterial blood pressure and neurologic outcome after resuscitation from cardiac arrest. Crit Care Med. 2014 Sep; 42(9):2083-91.
- The Hypothermia after Cardiac Arrest Study Group. Mild Therapeutic Hypothermia to Improve the Neurologic Outcome after Cardiac Arrest. N Engl J Med 2002; 346:549-56.
- Neilsen N, Wetterslev J, Cronberg T, et al. Targeted Temperature Management at 33°C versus 36°C after cardiac arrest. N Engl J Med. 2013.
- Perman SM, Kirkpatrick JN, Reitsma AM, et al. Timing of neuroprognostication in postcardiac arrest therapeutic hypothermia. Crit Care Med. 2012.
- Fugate JE, Wijdicks EF, Mandrekar J, et al. Predictors of neurologic outcome in hypothermia after cardiac arrest. Ann Neurol. 2010.