[tab_nav type=”two-up”][tab_nav_item title=”The Case” active=”true”][tab_nav_item title=”Answer” active=””][/tab_nav][tabs][tab active=”true”] A 54 year-old male IV drug abuser was recently admitted to the CCU for new onset CHF. He is found to have severe aortic regurgitation on his TTE and is subsequently found to have an evulsion of his left coronary cusp. The patient is being empirically treated for endocarditis and is awaiting a TEE.
He has been stable on the ventilator, so the RT places him on a pressure support mode and you get a call from the resident, who tells you the patient is really tachypnic and they need help managing the vent settings.
When you get to the room, you check the vent settings and this is what you see:
CSR from MarylandCCProject.org on Vimeo.
Question: What are should you be concerned about? What setting needs to be changed?
[/tab]
[tab]
Answer: This patient is experiencing Cheyne-Stokes respirations (CSR).
- Strongly consider getting a stat head CT with IV contrast/MRI to look for septic emboli or acute CVA
- Evaluate for worsening heart failure.
- The patient can be changed to a controlled ventilatory mode to better control gas exchange.
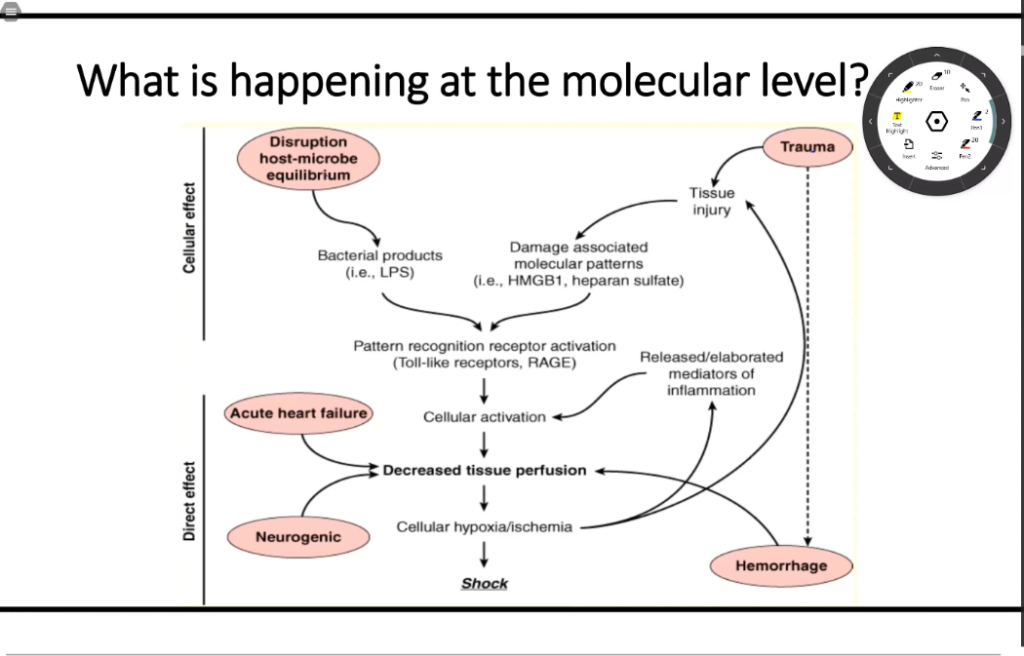
Cheyne-Stokes respirations are defined as a regular, recurring oscillation of the frequency and tidal volume of breathing followed by central apnea or hypopnea. It occurs as a result of instability in the feedback control system that regulates ventilation and minimizes oscillations on PaCO2 and PaO2.
Causes:
- Heart failure/severe LV dysfunction
- Stroke
- Central sleep apnea syndromes
Heart Failure: Can result in hypoxia and low cardiac output
- In patients with heart failure, the periodic cycle duration averages about 60 seconds, compared with only 35 seconds in patients with idiopathic central sleep apnea or high-altitude periodic breathing without heart failure.
- Following central apnea, the length of the subsequent ventilatory phase is directly proportional to the lung to peripheral chemoreceptor circulation time and inversely proportional to cardiac output. Increased pulmonary vascular congestion and hypoxia can also provoke CSR.
Stroke: The cerebral cortex has an inhibitory action on respiratory reflexes.
- CSR occur in up to 50% of patients with supratententorial strokes, but can also occur after infratentorial strokes.
- Up to 26% of patients have recurrent central apneas in the first 24 hours after a stroke
- CSR and recurrent tend to diminish as patients become stable.
Cheyne-Stokes Respirations Resolved from MarylandCCProject.org on Vimeo.
References