[tab_nav type=”two-up”][tab_nav_item title=”Clinical Case” active=”true”][tab_nav_item title=”Answer” active=””][/tab_nav][tabs][tab active=”true”]
A 32 yo F s/p a tricuspid valve replacement secondary to MSSA endocarditis 8 months earlier presents with a one month history of dypsnea, fatigue, chills, sweats and fevers. Patient was originally seen at an OSH where, despite several negative blood cultures and a lack of splinter hemorrhages, Osler nodes or Janeway lesions, she was started on empiric antibiotics and transferred to the University of Maryland for evaluation.
On arrival to the Emergency Department she appears to be extremely comfortable and in absolutely no distress. She is pacing about the room, laughing and talking on her phone. She had only a mild cough and diaphoresis.
On arrival the following Parasternal Long View was obtained:
With further rotation, the Right Ventricle was better visualized:
Of note, there was a mass entering the Right Ventricle, so the probe was rotated and a Parasternal Short View was obtained at the level of the mitral valve:
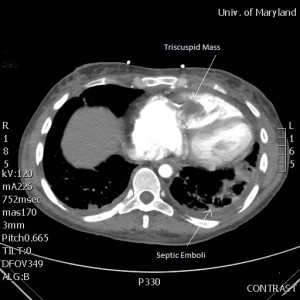
A CT Angiogram further revealed multiple punctate emboli as well as visualizing a mass on the tricuspid valve:
With the diagnosis Recurrent Tricuspid Endocarditis Cardiothoracic surgery was consulted. However, due to her continued IVDA and noncompliance, they refused any surgical intervention. A formal evaluation of her cardiac function shows that the left side of her heart is functioning normally, and her pulmonary status is stable. The EM intern ordered cardiac enzymes and a BNP, all of which are WNL.
The question is: What do you do now?
[/tab][tab]
1) Early, broad spectrum antibiotics with guidance from microbiological testing
- Up to 31% of blood cultures are negative in endocarditis, mostly due to either previous antibiotic treatment or infection with obligate intracellular bacteria, fungus or fastidious pathogens
- Taking 2 sets of 2 blood culture sets, separated by 2 hours is recommended to further the diagnostic yield
2) Early surgical management is the only definitive cure, with mortality directly correlated to the degree of heart failure, however……
- The current AHA guidelines recommend medical therapy for endocarditis associated with IVDA due to the 1% to 5% risk of recurrence per year
- Recurrent pulmonary emboli are not an indication for tricuspid valve replacement unless fever persists beyond 3 weeks of antibiotic therapy in the absence of a pulmonary abscess
3) Currently, there is no validated risk score that is correlated to increased mortality. Studies show that elevated BNP and troponin can be used as surrogate predictors of outcome.
Case Conclusion: The patient was admitted to the ICU when she decompensated. However, with aggressive, early antibiotics and symptom control, she was extubated within 10 days and was eventually discharged with IV antibiotics. She developed no left-sided cardiac dysfunction and thus she required no emergent operative intervention. It is hoped that with cessation of IVDA she will eventually be a candidate for elective repair.
Suggested Reading
[/tab][/tabs]